Non-Insured Health Benefits Program: First Nations and Inuit Health Branch: Annual Report 2016-2017
On this page
- Section 1: Introduction
- Section 2: Client Population
- Section 3: NIHB Program Benefit Expenditures
- Section 4: NIHB Pharmacy Expenditure and Utilization Data
- Section 5: NIHB Dental Expenditure and Utilization Data
- Section 6: NIHB Medical Transportation Expenditure and Utilization Data
- Section 7: NIHB Vision Benefits, Mental Health Counselling Benefits and Other Health Care Benefits Data
- Section 8: Regional Expenditure Trends 2007/08 to 2016/17
- Section 9: NIHB Program Administration
- Section 10: NIHB Policy and program initiatives
Section 1: Introduction
During 2016/17, the Non-Insured Health Benefits (NIHB) Program of the First Nations and Inuit Health Branch (FNIHB) at the Department of Indigenous Services Canada provided 853,088 eligible First Nations and Inuit clients with access to a range of medically necessary health-related goods and services not otherwise provided through private insurance plans, provincial/territorial health or social programs.
The NIHB Program covers the following medically necessary benefits:
- Prescription and over-the-counter drugs;
- Medical supplies and equipment;
- Dental care;
- Vision care;
- Mental health counselling; and
- Medical transportation to access health services not available locally.
Through the coverage of these benefits, the Department of Indigenous Services Canada supports First Nations and Inuit in reaching an overall health status that is comparable with other Canadians.
The NIHB Program operates according to the following guiding principles:
- All registered First Nations and recognized Inuit normally resident of Canada, and not otherwise covered under a separate agreement with federal or provincial governments or through a separate self-government agreement, are eligible for non-insured health benefits, regardless of location in Canada or income level;
- Benefits will be provided based on professional, medical or dental judgment, consistent with the best practices of health services delivery and evidence-based standards of care;
- There will be national consistency with respect to benefit coverage and access;
- The Program will be managed in a sustainable and cost-effective manner;
- Management processes will be transparent and involve collaboration with First Nations and Inuit organizations; and
- When an NIHB-eligible client is also covered by another public or private health care plan, claims must be submitted to the client's other health care/benefits plan first. NIHB will then coordinate payment with the other plan on eligible benefits.
Now in its twenty-third edition, the 2016/17 NIHB Annual Report provides national and regional data on the NIHB Program client population, expenditures, benefit types and benefit utilization. This Report is published in accordance with the NIHB Program's performance management responsibilities and is intended for the following target audiences:
- First Nations and Inuit organizations and governments at community, regional and national levels;
- Regional and Headquarters managers and staff of Health Canada; and
- Others in government and in non-government organizations with an interest in the provision of health services to First Nations and Inuit communities
British Columbia Tripartite Agreement
The British Columbia Tripartite Framework Agreement on First Nation Health Governance was signed by Canada, the First Nations Health Council (FNHC) and the British Columbia Ministry of Health on October 13, 2011. A key commitment made in the Framework Agreement is the transfer of Federal Health Programs, including Non-Insured Health Benefits (NIHB), from Canada to the First Nations Health Authority (FNHA).
Between July 2nd, 2013 and October 1st, 2013, the FNHA assumed responsibility for the design, planning, management and delivery of the Non-Insured Health Benefits Program to First Nations clients residing in the British Columbia Region. The Department of Indigenous Services Canada has established and implemented measures so that Inuit clients, and First Nations who are in British Columbia temporarily, will continue to access benefits through the federal NIHB Program.
As a transitional measure, The Department of Indigenous Services Canada has continued to provide claims processing and certain adjudication services for the Pharmacy, Dental and MS&E benefits to First Nations clients in British Columbia on behalf of the FNHA. This arrangement will be in place for a term of up to four years. During 2016/17, the NIHB program and the FNHA continued working together in support of ongoing capacity building and to prepare for the full transfer of the NIHB Program in British Columbia following the conclusion of this transition period.
Section 2: Client Population
As of March 31, 2017, there were 853,088 First Nations and Inuit clients eligible to receive benefits under the NIHB Program. The NIHB client population decreased significantly in 2013/14 as a result of the creation of the First Nations Health Authority (FNHA). In a phased approach, between July and October 2013, the FNHA assumed the programs, services, and responsibilities formerly delivered by the Department of Indigenous Services Canada's First Nations and Inuit Health Branch (FNIHB) to First Nation clients residing in British Columbia. Of the 853,088 total eligible clients at the end of the 2016/17 fiscal year, 806,117 (94.5%) were First Nations clients while 46,971 (5.5%) were Inuit clients.
To be an eligible client of the NIHB Program, an individual must be a resident of Canada and have the following status:
- A registered Indian according to the Indian Act; or
- An Inuk recognized by one of the Inuit Land Claim organizations; or
- An infant less than one year of age, whose parent is an eligible client; and
- Currently registered, or eligible for registration, under a provincial or territorial health insurance plan; and
- Is not otherwise covered under a separate agreement (e.g., a self-government agreement) with federal, provincial or territorial governments.
First Nations and Inuit population data are drawn from the Status Verification System (SVS) which is operated by FNIHB. SVS data on First Nations clients are based on information provided by Crown-Indigenous Relations and Northern Affairs Canada (CIRNA). SVS data on Inuit clients are based on information provided by the Governments of the Northwest Territories and Nunavut, and Inuit organizations including the Inuvialuit Regional Corporation, Nunavut Tunngavik Incorporated and the Makivik Corporation.
Historically, the First Nations and Inuit population has a higher growth rate than the Canadian population as a whole. This is primarily because First Nations and Inuit have a higher birth rate compared to the overall Canadian population. In addition, amendments to the Indian Acthave meant that a greater numbers of individuals are able to claim or restore their status as registered Indians. The passage of Bill C-3, the Gender Equity in Indian Registration Act, which came into force on January 31, 2011, has given eligible grandchildren of women who lost status as a result of marrying non-Indian men, entitlement to become registered as an Indian in accordance with the Indian Act. Once registered under the Indian Act, these individuals will be eligible to receive benefits through the NIHB Program. As of March 31, 2017, a total of 29,664 clients had become eligible to receive benefits through the NIHB Program as a result of this legislation.
The creation of the new Qalipu Mi'kmaq First Nations band was announced on September 26, 2011 as a result of a settlement agreement that was negotiated between the Government of Canada and the Federation of Newfoundland Indians (FNI). Through the formation of this band, members of the Qalipu Mi'kmaq became recognized under the Indian Act and eligible for registration. As of March 31, 2017, a total of 24,745 Qalipu clients were registered in the SVS and were eligible to receive benefits through the NIHB Program.
Figure 2.1: Eligible Client Population by Region
March 2017
The total number of NIHB-eligible clients at the end of March 2017 was 853,088, an increase of 1.7% from March 2016.
The Ontario Region had the largest proportion of the eligible population, representing 24.3% of the national total, followed by the Manitoba Region at 17.9% and the Saskatchewan Region at 17.5%.
Note that Figure 2.1 lists population values based on region of band registration, which is not necessarily the client's current region of residence. The majority of British Columbia clients previously covered by the NIHB Program are now covered by the B.C. First Nation Health Authority (FNHA) and are not represented in this chart. The remaining NIHB clients in B.C. are Inuit clients, or clients associated with B.C. bands, but residing in other provinces and territories of Canada (where they are covered under the federal NIHB Program).
Figure 2.1: Eligible Client Population by Region
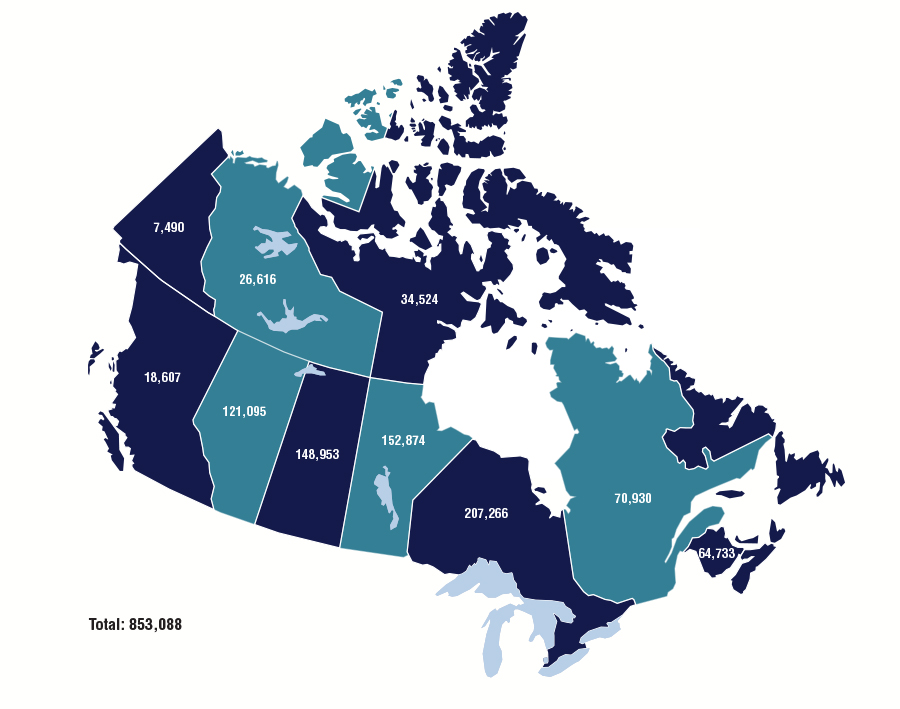
Total: 853,088
Source: SVS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Region | Totals |
|---|---|
| Atlantic | 64,733 |
| Quebec | 70,930 |
| Ontario | 207,266 |
| Manitoba | 152,874 |
| Saskatchewan | 148,953 |
| Alberta | 121,095 |
| British Columbia | 18,607 |
| Yukon | 7,490 |
| N.W.T. | 26,616 |
| Nunavut | 34,524 |
| Total: | 853,088 |
Figure 2.2: Eligible Client Population by Type and Region
March 2016 and March 2017
Of the 853,088 total eligible clients at the end of the 2016/17 fiscal year, 806,117 (94.5%) were First Nations clients while 46,971 (5.5%) were Inuit clients. The number of First Nations clients increased by 1.6% and the number of Inuit clients increased by 2.2%
From March 2016 to March 2017, Alberta had the highest percentage change in total eligible clients with a 2.5% increase, followed by Nunavut and Saskatchewan with increases of 2.4% and 2.0% respectively.
| Region | First Nations | Inuit | Total | % Change | |||
|---|---|---|---|---|---|---|---|
| March/16 | March/17 | March/16 | March/17 | March/16 | March/17 | 2016 to 2017 | |
| Atlantic | 63,362 | 64,362 | 350 | 371 | 63,712 | 64,733 | 1.6% |
| Quebec | 68,384 | 69,494 | 1,374 | 1,436 | 69,758 | 70,930 | 1.7% |
| Ontario | 203,517 | 206,501 | 715 | 765 | 204,232 | 207,266 | 1.5% |
| Manitoba | 150,277 | 152,667 | 198 | 207 | 150,475 | 152,874 | 1.6% |
| Saskatchewan | 145,899 | 148,879 | 69 | 74 | 145,968 | 148,953 | 2.0% |
| Alberta | 117,561 | 120,466 | 609 | 629 | 118,170 | 121,095 | 2.5% |
| B.C. | 18,938 | 18,258 | 339 | 349 | 19,277 | 18,607 | -3.5% |
| Yukon | 7,350 | 7,375 | 106 | 115 | 7,456 | 7,490 | 0.5% |
| N.W.T. | 17,899 | 18,115 | 8,468 | 8,501 | 26,367 | 26,616 | 0.9% |
| Nunavut | 0 | 0 | 33,714 | 34,524 | 33,714 | 34,524 | 2.4% |
| National | 793,187 | 806,117 | 44,733 | 46,971 | 839,129 | 853,088 | 1.7% |
| Source: SVS adapted by Business Support, Audit and Negotiations Division | |||||||
Figure 2.3: Eligible Client Population
Over the past 10 years, the total number of eligible clients in the SVS has increased by 6.7%, from 799,213 in March 2008 to 853,088 in March 2017.
The NIHB Program client population was significantly impacted during this period by amendments to the Indian Act, such as the passage of Bill C-31, Bill C-3, and the creation of the new Qalipu Mi'kmaq Band, which increased the NIHB client population. In contrast, the creation of the First Nations Health Authority (FNHA) in British Columbia and the settlement of First Nations and Inuit self-government agreements, such as those with the Nisga'a Lisims Government and the Nunatsiavut Government, have decreased the total NIHB client population, as these individuals no longer receive benefits through Indigenous Services Canada's NIHB Program. The most notable such change occurred in 2013-14, when approximately 133,430 clients in BC were removed from the NIHB client population when they became eligible to receive non-insured health benefits through the FNHA.
Figure 2.3.1: Eligible Client Population, March 2008 to March 2017
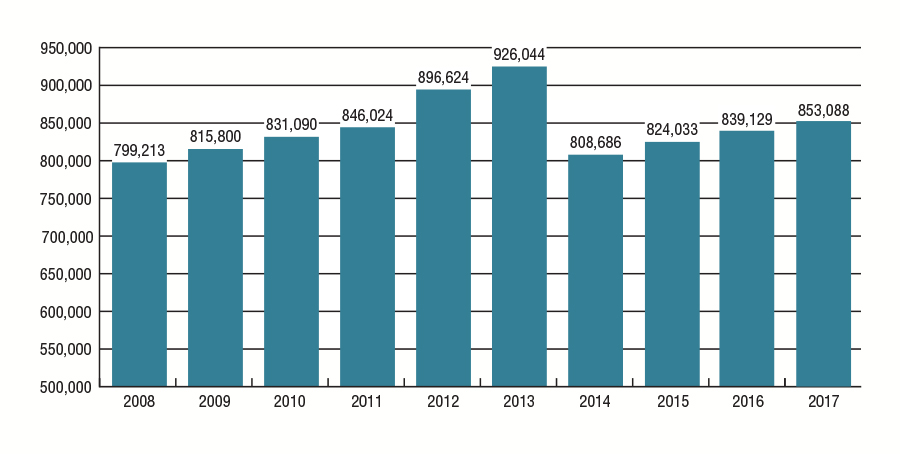
Source: SVS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Year | Totals |
|---|---|
| 2008 | 799,213 |
| 2009 | 815,800 |
| 2010 | 831,090 |
| 2011 | 846,024 |
| 2012 | 896,624 |
| 2013 | 926,044 |
| 2014 | 808,686 |
| 2015 | 824,033 |
| 2016 | 839,129 |
| 2017 | 853,088 |
Over the past five years, the NIHB Program's total number of eligible clients decreased by 7.9% from 926,044 in March 2013 to 853,088 in March 2017. Nunavut had the largest increase in eligible clients over this period, with a growth rate of 8.6%. The regions of Quebec, Manitoba, and Ontario followed with growth rates of 7.6%, 5.6% and 5.2% respectively.
| Region | March 2013 | March 2014 | March 2015 | March 2016 | March 2017 |
|---|---|---|---|---|---|
| Atlantic | 62,030 | 62,015 | 62,756 | 63,712 | 64,733 |
| Quebec | 65,944 | 66,819 | 68,274 | 69,758 | 70,930 |
| Ontario | 197,019 | 197,092 | 200,518 | 204,232 | 207,266 |
| Manitoba | 144,748 | 144,416 | 147,932 | 150,475 | 152,874 |
| Saskatchewan | 142,056 | 140,164 | 143,228 | 145,968 | 148,953 |
| Alberta | 115,867 | 113,590 | 115,886 | 118,170 | 121,095 |
| B.C. | 131,782 | 19,628 | 19,283 | 19,277 | 18,607 |
| Yukon | 8,682 | 7,138 | 7,402 | 7,456 | 7,490 |
| N.W.T. | 26,125 | 25,434 | 25,587 | 26,367 | 26,616 |
| Nunavut | 31,791 | 32,390 | 33,167 | 33,714 | 34,524 |
| Total | 926,044 | 808,686 | 824,033 | 839,129 | 853,088 |
| Annual % Change | 3.3% | -12.7% | 1.9% | 1.8% | 1.7% |
| Source: SVS adapted by Business Support, Audit and Negotiations Division | |||||
Figure 2.4: Annual Population Growth, Canadian Population and Eligible Client Population
2008 to 2017
From 2008 to 2017, the Canadian population increased by 10.5% while the NIHB eligible First Nations and Inuit client population increased by 6.7%. Prior to the removal of First Nations Health Authority (FNHA) clients, the NIHB ten year eligible population increase was 24.4%, with an average annual growth of 2.4%. Population growth is expected to return to historical rates in future fiscal years as the transition of residents of British Columbia to the FNHA is completed.
The higher than average NIHB Program client population growth rate of 6.0% in 2011-12 and 3.3% in 2012/13 can be attributed to the registration of new Bill C-3 clients as status Indians, and to new Qalipu Mi'kmaq First Nations clients in the Atlantic Region.
Figure 2.4: Annual Population Growth, Canadian Population and Eligible Client Population 2007 to 2016
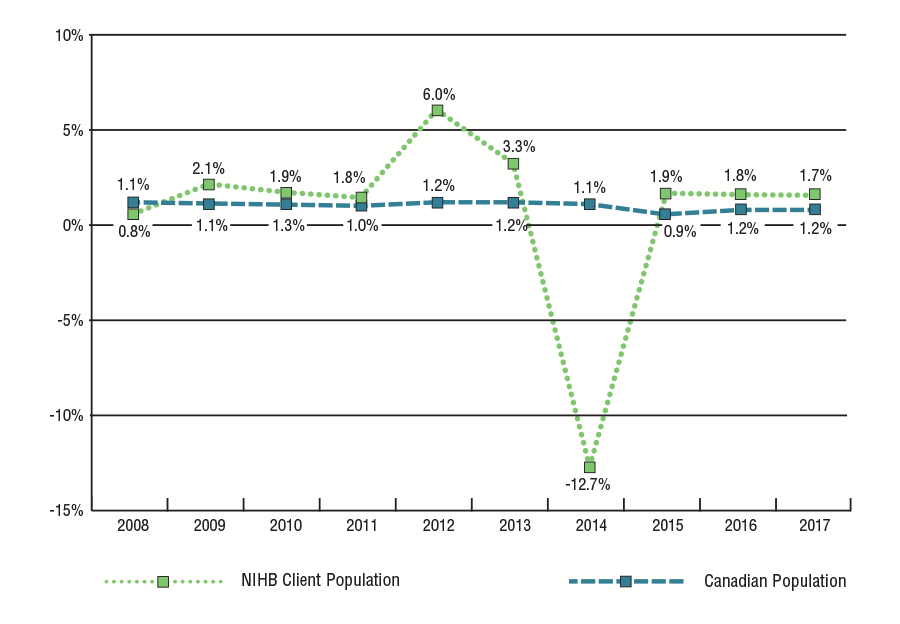
Source: SVS and Statistics Canada Catalogue No. 91-002-XWE, Quarterly Demographic Statistics, adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Year | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|---|---|---|
| NIHB Client Population | 0.8% | 2.1% | 1.9% | 1.8% | 6.0% | 3.3% | -12.7% | 1.9% | 1.8% | 1.7% |
| Canadian Population | 1.1% | 1.1% | 1.3% | 1.0% | 1.2% | 1.2% | 1.1% | 0.9% | 1.2% | 1.2% |
Figure 2.5: Eligible Client Population by Age Group, Gender and Region
March 2017
Of the 853,088 NIHB eligible clients on the SVS as of March 31, 2017, 49.2% were male (419,787) and 50.8% were female (433,301).
The average age of the eligible client population was 33 years of age. By region, this average ranged from a low of 27 years of age in Nunavut to a high of 38 years of age in the Yukon.
The average age of the male and female eligible client population was 32 years and 34 years respectively. The average age for males ranged from a low of 26 years in Nunavut to a high of 36 years in the Quebec and Yukon Region. The average age for females varied from a low of 27 years in Nunavut to a high of 39 years in the Yukon and Quebec Region.
The NIHB eligible First Nations and Inuit client population is relatively young with nearly two-thirds (64.8%) under the age of 40. Of the total population, almost one-third (32.8%) are under the age of 20.
The senior population (clients 65 years of age and over) has been slowly increasing as a proportion of the total NIHB client population. In 2007/08, seniors represented 5.9% of the overall NIHB population. Most recently in 2016/17, seniors accounted for 7.8%. This demographic trend will contribute to cost pressures on the NIHB Program.
| Region | Atlantic | Quebec | Ontario | Manitoba | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age Group | Male | Female | Total | Male | Female | Total | Male | Female | Total | Male | Female | Total |
| 0-4 | 1,462 | 1,442 | 2,904 | 1,779 | 1,660 | 3,439 | 4,683 | 4,600 | 9,283 | 5,577 | 5,276 | 10,853 |
| 5-9 | 2,265 | 2,193 | 4,458 | 2,639 | 2,529 | 5,168 | 7,438 | 7,204 | 14,642 | 8,357 | 8,193 | 16,550 |
| 10-14 | 2,605 | 2,508 | 5,113 | 2,615 | 2,362 | 4,977 | 7,781 | 7,328 | 15,109 | 7,836 | 7,604 | 15,440 |
| 15-19 | 2,685 | 2,614 | 5,299 | 2,588 | 2,516 | 5,104 | 8,111 | 7,854 | 15,965 | 7,483 | 7,020 | 14,503 |
| 20-24 | 2,893 | 2,862 | 5,755 | 2,982 | 2,877 | 5,859 | 9,028 | 8,786 | 17,814 | 7,613 | 7,379 | 14,992 |
| 25-29 | 2,726 | 2,627 | 5,353 | 2,799 | 2,749 | 5,548 | 8,605 | 8,431 | 17,036 | 6,947 | 6,903 | 13,850 |
| 30-34 | 2,397 | 2,351 | 4,748 | 2,395 | 2,465 | 4,860 | 7,560 | 7,389 | 14,949 | 5,587 | 5,393 | 10,980 |
| 35-39 | 2,186 | 2,202 | 4,388 | 2,248 | 2,208 | 4,456 | 6,814 | 7,086 | 13,900 | 4,782 | 4,586 | 9,368 |
| 40-44 | 2,131 | 2,173 | 4,304 | 2,139 | 2,225 | 4,364 | 6,650 | 6,707 | 13,357 | 4,436 | 4,477 | 8,913 |
| 45-49 | 2,254 | 2,285 | 4,539 | 2,327 | 2,440 | 4,767 | 6,834 | 7,135 | 13,969 | 4,471 | 4,690 | 9,161 |
| 50-54 | 2,134 | 2,269 | 4,403 | 2,388 | 2,703 | 5,091 | 7,076 | 7,493 | 14,569 | 4,072 | 4,194 | 8,266 |
| 55-59 | 1,828 | 2,150 | 3,978 | 2,260 | 2,549 | 4,809 | 6,216 | 7,067 | 13,283 | 3,174 | 3,502 | 6,676 |
| 60-64 | 1,442 | 1,805 | 3,247 | 1,688 | 2,167 | 3,855 | 4,654 | 5,775 | 10,429 | 2,143 | 2,557 | 4,700 |
| 65+ | 2,695 | 3,549 | 6,244 | 3,441 | 5,192 | 8,633 | 9,277 | 13,684 | 22,961 | 3,732 | 4,890 | 8,622 |
| Total | 31,703 | 33,030 | 64,733 | 34,288 | 36,642 | 70,930 | 100,727 | 207,266 | 204,232 | 76,210 | 76,664 | 152,874 |
| Average Age | 35 | 37 | 36 | 36 | 39 | 37 | 35 | 37 | 36 | 29 | 31 | 30 |
| Source: SVS adapted by Business Support, Audit and Negotiations Division | ||||||||||||
| Region | Saskatchewan | Alberta | B.C. | Yukon | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age Group | Male | Female | Total | Male | Female | Total | Male | Female | Total | Male | Female | Total |
| 0-4 | 4,956 | 4,796 | 9,752 | 4,362 | 4,215 | 8,577 | 900 | 906 | 1,806 | 143 | 124 | 267 |
| 5-9 | 8,145 | 7,844 | 15,989 | 6,866 | 6,572 | 13,438 | 585 | 577 | 1,162 | 268 | 210 | 478 |
| 10-14 | 7,704 | 7,618 | 15,322 | 6,308 | 6,151 | 12,459 | 589 | 579 | 1,168 | 242 | 230 | 472 |
| 15-19 | 7,364 | 7,289 | 14,653 | 5,897 | 5,609 | 11,506 | 664 | 627 | 1,291 | 288 | 266 | 554 |
| 20-24 | 7,589 | 7,412 | 15,001 | 6,258 | 5,770 | 12,028 | 741 | 593 | 1,334 | 309 | 298 | 607 |
| 25-29 | 7,195 | 7,016 | 14,211 | 5,576 | 5,441 | 11,017 | 738 | 665 | 1,403 | 315 | 310 | 625 |
| 30-34 | 5,827 | 5,765 | 11,592 | 4,735 | 4,593 | 9,328 | 733 | 706 | 1,439 | 312 | 278 | 590 |
| 35-39 | 4,898 | 4,775 | 9,673 | 3,836 | 3,973 | 7,809 | 670 | 671 | 1,341 | 273 | 237 | 510 |
| 40-44 | 4,332 | 4,505 | 8,837 | 3,371 | 3,521 | 6,892 | 599 | 609 | 1,208 | 241 | 222 | 463 |
| 45-49 | 4,268 | 4,466 | 8,734 | 3,289 | 3,431 | 6,720 | 628 | 651 | 1,279 | 307 | 251 | 558 |
| 50-54 | 3,670 | 3,983 | 7,653 | 2,915 | 3,262 | 6,177 | 535 | 712 | 1,247 | 327 | 325 | 652 |
| 55-59 | 2,887 | 3,245 | 6,132 | 2,308 | 2,677 | 4,985 | 461 | 665 | 1,126 | 267 | 306 | 573 |
| 60-64 | 1,884 | 2,247 | 4,131 | 1,573 | 2,022 | 3,595 | 306 | 467 | 773 | 164 | 215 | 379 |
| 65+ | 3,053 | 4,220 | 7,273 | 2,676 | 3,888 | 6,564 | 736 | 1,294 | 2,030 | 296 | 466 | 762 |
| Total | 73,722 | 75,181 | 148,953 | 59,970 | 61,125 | 121,095 | 8,885 | 9,722 | 18,607 | 3,752 | 3,738 | 7,490 |
| Average Age | 29 | 30 | 29 | 29 | 30 | 30 | 33 | 37 | 35 | 36 | 39 | 38 |
| Source: SVS adapted by Business Support, Audit and Negotiations Division | ||||||||||||
| Region | N.W.T. | Nunavut | TOTAL | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Age Group | Male | Female | Total | Male | Female | Total | Male | Female | Total |
| 0-4 | 654 | 641 | 1,295 | 2,044 | 1,909 | 3,953 | 26,560 | 25,569 | 52,129 |
| 5-9 | 1,036 | 966 | 2,002 | 2,071 | 2,038 | 4,109 | 39,670 | 38,326 | 77,996 |
| 10-14 | 988 | 1,001 | 1,989 | 1,915 | 1,787 | 3,702 | 38,583 | 37,168 | 75,751 |
| 15-19 | 989 | 983 | 1,972 | 1,742 | 1,645 | 3,387 | 37,811 | 36,423 | 74,234 |
| 20-24 | 1,384 | 1,329 | 2,713 | 1,626 | 1,578 | 3,204 | 40,423 | 38,884 | 79,307 |
| 25-29 | 1,356 | 1,368 | 2,724 | 1,593 | 1,540 | 3,133 | 37,850 | 37,050 | 74,900 |
| 30-34 | 1,111 | 1,016 | 2,127 | 1,212 | 1,225 | 2,437 | 31,869 | 31,181 | 63,050 |
| 35-39 | 923 | 922 | 1,845 | 998 | 1,011 | 2,009 | 27,628 | 27,671 | 55,299 |
| 40-44 | 785 | 851 | 1,636 | 871 | 881 | 1,752 | 25,555 | 26,171 | 51,726 |
| 45-49 | 946 | 993 | 1,939 | 927 | 944 | 1,871 | 26,251 | 27,286 | 53,537 |
| 50-54 | 825 | 910 | 1,735 | 771 | 809 | 1,580 | 24,713 | 26,660 | 51,373 |
| 55-59 | 653 | 779 | 1,432 | 539 | 557 | 1,096 | 20,593 | 23,497 | 44,090 |
| 60-64 | 420 | 571 | 991 | 370 | 377 | 747 | 14,644 | 18,203 | 32,847 |
| 65+ | 992 | 1,224 | 2,216 | 739 | 805 | 1,544 | 27,637 | 39,212 | 66,849 |
| Total | 13,062 | 13,554 | 26,616 | 17,418 | 17,106 | 34,524 | 419,787 | 433,301 | 853,088 |
| Average Age | 33 | 35 | 34 | 26 | 27 | 27 | 32 | 34 | 33 |
| Source: SVS adapted by Business Support, Audit and Negotiations Division | |||||||||
Figure 2.6: Population Analysis by Age Group
The overall First Nations and Inuit client population is relatively young compared to the general Canadian population. The share of the NIHB client population under 20 years of age was 32.8% compared to 21.6% of the same age group in the Canadian population. The average age of First Nations and Inuit clients is 33 compared to 41 years of age for the Canadian population.
Figure 2.6.1: Proportion of Canadian Population and of the First Nations and Inuit (FN&I) Client Population by Age Group
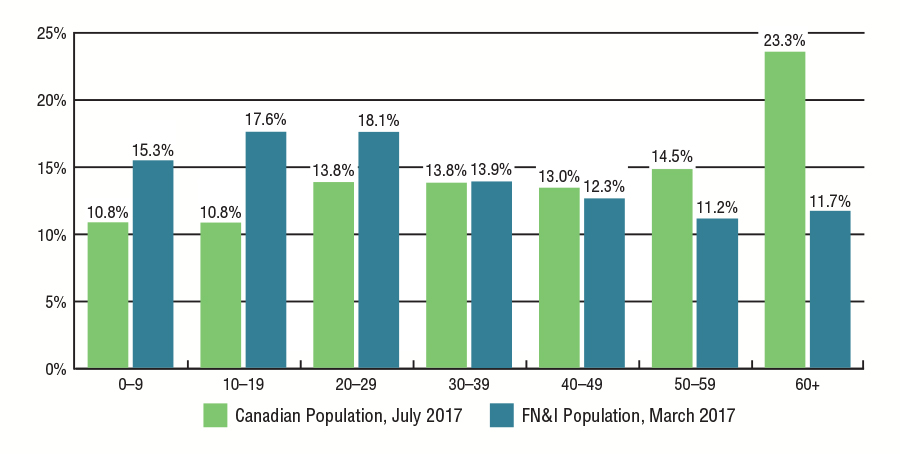
Source: SVS and Statistics Canada CANSIM table 051-0001, Population by Age and Sex Group, adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Age Group | Canadian Population, July 2017 | FN&I Population, March 2017 |
|---|---|---|
| 0-9 | 10.8% | 15.3% |
| 10-19 | 10.8% | 17.6% |
| 20-29 | 13.8% | 18.1% |
| 30-39 | 13.8% | 13.9% |
| 40-49 | 13.0% | 12.3% |
| 50-59 | 14.5% | 11.2% |
| 60+ | 23.3% | 11.7% |
A comparison of March 2013 to March 2017 eligible client population shows an aging population. The client population 40 and above, as a proportional share of the overall client population, increased from 34.4% in 2013 to 35.2% in 2017.
As the First Nations and Inuit client population ages, the costs associated with delivering Non-Insured Health Benefits, particularly pharmacy benefits, to this client population are expected to increase significantly.
Figure 2.6.2: Proportion of Eligible First Nations and Inuit Client Population by Age Group
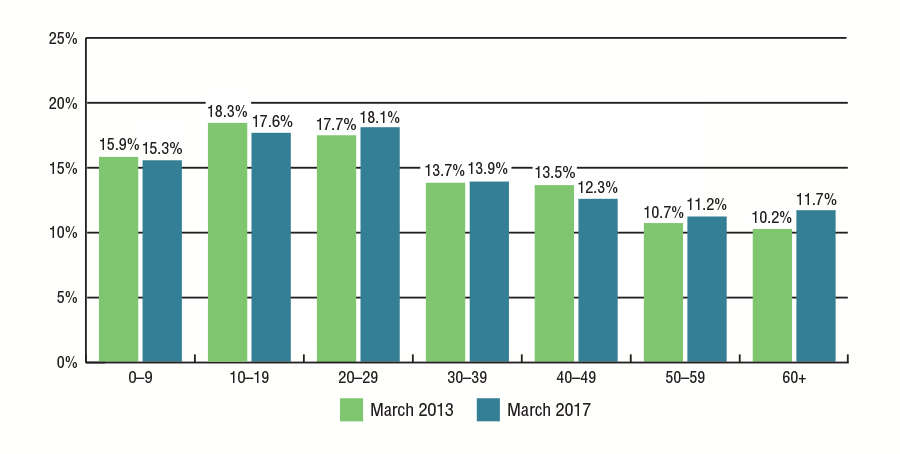
Source: SVS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Age Group | March 2013 | March 2017 |
|---|---|---|
| 0-9 | 15.9% | 15.3% |
| 10-19 | 18.3% | 17.6% |
| 20-29 | 7.7% | 18.1% |
| 30-39 | 13.7% | 13.9% |
| 40-49 | 13.5% | 12.3% |
| 50-59 | 10.7% | 11.2% |
| 60+ | 10.2% | 11.7% |
Section 3: NIHB Program Benefit Expenditures
Figure 3.1: NIHB Program Sustainability
2016/17
Cost and service pressures on the Canadian health system have been linked to factors such as an aging population and the increased demand for and utilization of health goods, particularly pharmaceuticals, and services. In addition to these factors, NIHB Program expenditures are driven by the number of eligible clients and their medical needs. The NIHB client population is growing at approximately two times the Canadian population growth rate. A significant proportion of NIHB clients live in small and remote communities, and require medical transportation to access health services that are not available locally.
| Client Base | Market Forces | Clinical Evidence |
|---|---|---|
|
|
|
Figure 3.2: NIHB Expenditures by Benefit ($ Millions)
2016/17
In 2016/17, total NIHB Program benefit expenditures were $1,207.5 million. This represents an increase of 9.7% over NIHB expenditures of $1,100.5 million in 2015/16.
Of the 2016/17 total, Pharmacy costs (including medical supplies and equipment) represented the largest proportion at $494.5 million (41.0%), followed by Medical Transportation costs at $417.0 million (34.5%) and Dental costs at $235.8 million (19.5%).
Figure 3.2: NIHB Expenditures by Benefit ($ Millions) 2016/17
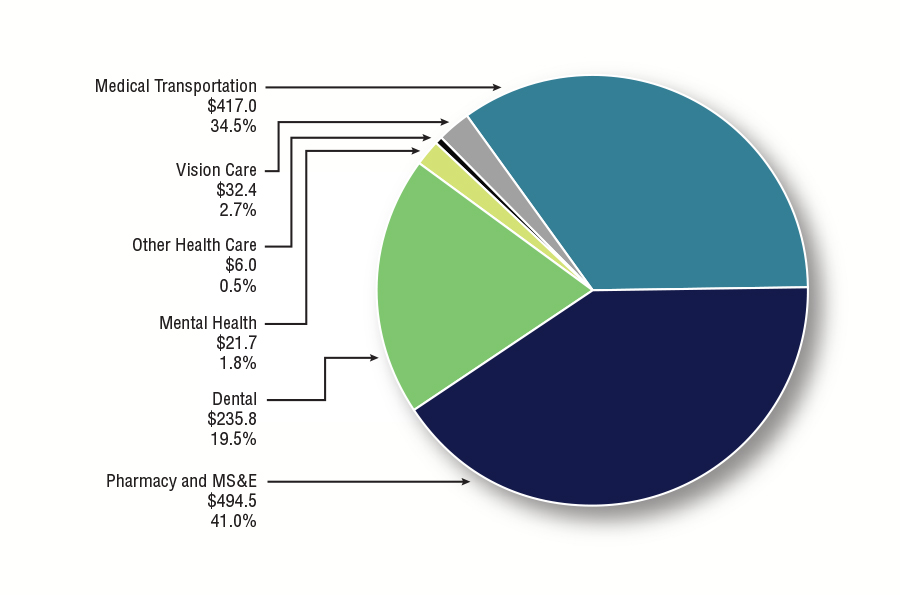
Text Equivalent
| Benefit | Expenditure in millions | proportion of total expenditure |
|---|---|---|
| Pharmacy and MS&E | $494.5 | 41.0% |
| Dental | $235.8 | 19.5% |
| Vision Care | $32.4 | 2.7% |
| Mental Health | $21.7 | 1.8% |
| Other Health Care | $6.0 | 0.5% |
| Medical Transportation | $417.0 | 34.5% |
| Total NIHB Program Benefit Expenditures | $1,207.5M | 100% |
* Not reflected in the $1,207.5 million in NIHB expenditures is approximately $37.2 million in administration costs including Program staff and other headquarters and regional costs. More detail is provided in Figure 11.1.
Figure 3.3: NIHB Expenditures and Growth by Benefit
2016/17
NIHB Program benefit expenditures increased by 9.7%, or $106.9 million overall from 2015/16. All NIHB benefit areas had an increase in expenditures over the previous fiscal year. The highest net increase in expenditures over fiscal year 2015/16 was in the NIHB Medical Transportation benefit at $41.1 million, followed by NIHB Pharmacy and MS&E benefits with an increase of $38.1 million and the NIHB Dental benefit which increased by $18.7 million. Factors affecting benefit expenditure growth are discussed in subsequent sections of this report.
| Benefit | Total Expenditures ($ 000's) 2015/16 | Total Expenditures ($ 000's) 2016/17 | % Change From 2015/16 |
|---|---|---|---|
| Medical Transportation | $375,904 | $417,035 | 10.9% |
| Pharmacy and MS&E | $456,430 | $494,520 | 8.3% |
| Dental | $217,109 | $235,831 | 8.6% |
| Vision Care | $30,017 | $32,370 | 7.8% |
| Mental Health | $16,193 | $21,728 | 34.2% |
| Other | $4,858 | $5,974 | 23.0% |
| Total Expenditures | $1,100,512 | $1,207,458 | 9.7% |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | |||
Figure 3.4: NIHB Expenditures by Benefit and Region ($ 000's)
2016/17
The Manitoba Region accounted for the highest proportion of total expenditures at $292.0 million, or 24.2% of the national total, followed by the Ontario Region at $231.7 million (19.2%), and the Saskatchewan Region at $220.4 million (18.2%). In comparison, the lowest expenditure was in the Atlantic Region at $55.1 million (4.6%).
Headquarters expenditures by benefit type represent costs paid for claims processing services. Headquarters expenditures in the 'Other Health Care' category include funding arrangements with the FNHA for Bill C-3 and Qalipu clients and for payment of Inuit premiums in British Columbia, as well as with national client stakeholder organizations (Assembly of First Nations and Inuit Tapiriit Kanatami), and regional Indigenous organizations. These expenditures account for 2.0% ($23.7 million) of NIHB expenditures, and do not include the $16.3 million in Headquarters administrative costs outlined in Figure 11.1.
| Region | Medical Transportation | Pharmacy | Dental | Vision Care | Mental Health | Other Health Care | TOTAL |
|---|---|---|---|---|---|---|---|
| Atlantic | $9,277 | $31,899 | $9,593 | $3,502 | $601 | $207 | $55,079 |
| Quebec | $23,501 | $47,444 | $17,569 | $1,762 | $1,292 | $263 | $91,831 |
| Ontario | $74,890 | $94,101 | $52,105 | $6,223 | $4,091 | $254 | $231,663 |
| Manitoba | $147,167 | $94,757 | $39,986 | $4,204 | $5,635 | $240 | $291,989 |
| Saskatchewan | $58,902 | $104,082 | $47,321 | $6,533 | $3,304 | $210 | $220,352 |
| Alberta | $48,157 | $77,265 | $44,315 | $6,928 | $6,444 | $0 | $183,108 |
| North | $55,125 | $28,488 | $21,966 | $3,217 | $362 | $260 | $109,417 |
| Headquarters | $16 | $16,302 | $2,877 | $0 | $0 | $4,540 | $23,735 |
| Total | $417,035 | $235,831 | 100% | $32,370 | $21,728 | $5,974 | $1,207,458 |
| Source: FIRMS adapted by by Business Support, Audit and Negotiations Division | |||||||
Figure 3.5: Proportion of NIHB Expenditures by Region
2016/17
In 2016/17, the Manitoba Region had the highest proportion of total NIHB expenditures (24.2%) and accounted for 35.3% of total NIHB Medical Transportation expenditures. This can be attributed to the large number of First Nations clients living in remote or fly-in only northern communities in the Manitoba Region.
The Saskatchewan Region accounted for the highest proportion of NIHB Pharmacy expenditures at 21.0%, followed closely by Manitoba and Ontario at 19.2% and 19.0% respectively.
The Ontario Region, which accounted for 19.2% of total NIHB expenditures in 2016/17, recorded the highest proportion of total NIHB Dental expenditures at 22.0%. This region also accounted for the highest proportion of the total NIHB population at 24.3%.
The proportion of NIHB Vision Care expenditures ranged from highs of 21.4% in the Alberta Region, 20.2% in the Saskatchewan Region and 19.2% in the Ontario Region to a low of 5.4 % in Quebec.
The Alberta Region (29.7%) and the Manitoba Region (25.9%) combined accounted for over one-half of total NIHB Mental Health expenditures in 2016/17.
| Region | Medical Transportation | Pharmacy | Dental | Vision Care | Mental Health | Other Health Care | Proportion of NIHB Expenditure | Proportion of NIHB Population |
|---|---|---|---|---|---|---|---|---|
| Atlantic | 2.2% | 6.5% | 4.1% | 10.8% | 2.8% | 3.5% | 4.6% | 7.6% |
| Quebec | 5.6% | 9.6% | 7.4% | 5.4% | 5.9% | 4.4% | 7.6% | 8.3% |
| Ontario | 18.0% | 19.0% | 22.0% | 19.2% | 18.8% | 4.3% | 19.2% | 24.3% |
| Manitoba | 35.3% | 19.2% | 16.9% | 13.0% | 25.9% | 4.0% | 24.2% | 17.9% |
| Saskatchewan | 14.1% | 21.0% | 20.0% | 20.2% | 15.2% | 3.5% | 18.2% | 17.5% |
| Alberta | 11.5% | 15.6% | 18.8% | 21.4% | 29.7% | 0.0% | 15.2% | 14.2% |
| North | 13.2% | 5.8% | 9.5% | 9.9% | 1.7% | 4.4% | 9.1% | 8.0% |
| Headquarters | 0.0% | 3.3% | 1.2% | 0.0% | 0.0% | 76.0% | 2.0% | 0.0% |
| Total | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% |
| Source: FIRMS and SVS adapted by by Business Support, Audit and Negotiations Division | ||||||||
Figure 3.6: Proportion of NIHB Regional Expenditures by Benefit
2016/17
At the national level, approximately three-quarters (75.5%) of total Program expenditures occurred in two benefit areas: pharmacy (41.0%) and medical transportation (34.5%). Dental expenditures accounted for one-fifth (19.5%) of total NIHB expenditures.
Medical Transportation expenditures accounted for half of benefit expenditures in the Manitoba and Northern Regions (50.1% and 50.4%, respectively). In the Atlantic Region, 16.9% of benefit expenditures were spent on medical transportation.
The proportion of dental expenditures ranged from 13.7% in the Manitoba Region to 24.2% in Alberta Region.
In the Atlantic Region, 57.9% of total expenditures were spent on pharmacy benefits. Pharmacy costs represented the highest percentage of total expenditures in all regions except in the Northern Region and in Manitoba, where transportation accounted for the largest share of costs.
| Region | Medical Transportation | Pharmacy | Dental | Vision Care | Mental Health | Other Health Care | Total |
|---|---|---|---|---|---|---|---|
| Atlantic | 16.8% | 57.9% | 17.4% | 6.4% | 1.1% | 0.4% | 100% |
| Quebec | 25.6% | 51.7% | 19.1% | 1.9% | 1.4% | 0.3% | 100% |
| Ontario | 32.3% | 40.6% | 22.5% | 2.7% | 1.8% | 0.1% | 100% |
| Manitoba | 50.4% | 32.5% | 13.7% | 1.4% | 1.9% | 0.1% | 100% |
| Saskatchewan | 26.7% | 47.2% | 21.5% | 3.0% | 1.5% | 0.1% | 100% |
| Alberta | 26.3% | 42.2% | 24.2% | 3.8% | 3.5% | 0.0% | 100% |
| North | 50.4% | 26.0% | 20.1% | 2.9% | 0.3% | 0.2% | 100% |
| Headquarters | 0.1% | 68.7% | 12.1% | 0.0% | 0.0% | 19.1% | 100% |
| National | 34.5% | 41.0% | 19.5% | 2.7% | 1.8% | 0.5% | 100% |
| Source: FIRMS and SVS adapted by by Business Support, Audit and Negotiations Division | |||||||
Figure 3.7: NIHB Annual Expenditures by Benefit ($ 000's)
2007/08 to 2016/17
In 2016/17, NIHB Program expenditures totalled $1,207.5 million, an increase of 9.7% from $1,100.5 million in 2015/16. Since 2007/08, total expenditures have grown by 34.4%. The annualized rate of growth over this period was 3.5%. There has been wide variation in growth rates between 2007/08 and 2016/17, with a low of -7.1% in 2013/14Footnote 1 to a high of 9.7% in 2016/17.
Fluctuations in NIHB expenditure growth rates are impacted by a number of factors. Changes in the eligible client population have a direct impact on growth. Notable examples include the transfer of responsibility for First Nations clients residing in BC to the FNHA in 2013/14, the creation of the Qalipu Mi'kmaq Band in 2011, and court decisions such as Bill C-3 that have resulted newly eligible clients.
NIHB expenditure growth rates are also impacted by the introduction of new therapies and generic drugs to the market, changes to provincial pricing policies, and economic inflationary pressures. In addition, rates of expenditure growth are impacted by new self-government initiatives, policy changes to improve access to benefits or promote sustainability, and changes in service delivery models within the Program, within the federal government, and between the provinces and territories.
NIHB Annual Expenditures ($ Millions) and Percentage Change

Source: FIRMS and SVS adapted by by Business Support, Audit and Negotiations Division
Text Equivalent
| BENEFIT | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|---|---|---|---|---|
| Annual Expenditures ($ Millions) | $898 | $940 | $989 | $1,028 | $1,074 | $1,105 | $1,1026 | $1,031 | $1,101 | $1,207 |
| Percentage Change | 4.9% | 4.7% | 5.2% | 3.9% | 4.5% | 2.8% | -7.1% | 0.5% | 6.7% | 9.7% |
Figure 3.8: NIHB Annual Expenditures by Benefit ($ 000's)
2007/08 to 2016/17
In the period from 2007/08 to 2016/17, expenditures for NIHB Medical Transportation and Dental benefits have grown more than other benefit areas. NIHB Medical Transportation expenditures grew by 59.0% from $262.3 million in 2007/08 to $417.0 million in 2016/17. NIHB Dental expenditures rose by 42.4% from $165.6 million in 2007/08 to $235.8 million in 2015/16.
Over the same period, NIHB Pharmacy expenditures increased by 22.6% and NIHB Vision expenditures had an increase of 26.3%.
NIHB Mental Health expenditures increased by 76.8% over this same time period from $12.3 million in 2007/08 to $21.7 million in 2016/17.
Decreases in 'Other' expenditures in 2009/10 and 2013/14 can be attributed to the Government of Alberta eliminating Alberta health care insurance premiums for all Alberta residents in 2009 and to the transfer of responsibility for health care insurance premiums for First Nations clients residing in British Columbia to the First Nations Health Authority (FNHA) in 2013. This expenditure category also includes funding arrangements with the FNHA for Bill C-3 and Qalipu clients and for payment of premiums for Inuit clients in British Columbia, as well as with regional Indigenous organizations that employ NIHB Navigators to act as a resource for communities, organizations or individuals who need assistance or information on the NIHB Program.
| Benefit | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|---|---|---|---|---|
| Medical Transportation | $262,294 | $280,446 | $301,673 | $311,760 | $333,304 | $351,424 | $352,036 | $357,963 | $375,904 | $417,035 |
| Pharmacy | $403,248 | $418,968 | $435,097 | $440,768 | $459,359 | $462,699 | $416,165 | $422,350 | $456,430 | $494,520 |
| Dental | $165,576 | $176,382 | $194,918 | $215,796 | $219,057 | $222,706 | $207,179 | $201,886 | $217,109 | $235,831 |
| Vision Care | $25,621 | $26,577 | $27,779 | $29,219 | $29,780 | $32,167 | $31,459 | $29,704 | $30,017 | $32,370 |
| Mental Health | $12,289 | $11,380 | $12,516 | $12,083 | $12,936 | $14,337 | $14,152 | $15,581 | $16,193 | $21,728 |
| Other | $29,211 | $26,430 | $17,110 | $18,428 | $19,868 | $21,257 | $5,406 | $4,005 | $4,858 | $5,974 |
| Total | $898,239 | $940,182 | $989,094 | $1,028,053 | $1,074,304 | $1,074,591 | $1,026,397 | $1,031,488 | $1,100,512 | $1,207,458 |
| Annual % Change | 4.9% | 4.7% | 5.2% | 3.9% | 4.5% | 2.8% | -7.1% | 0.5% | 6.7% | 9.7% |
| Source: FIRMS adapted by by Business Support, Audit and Negotiations Division | ||||||||||
Figure 3.9: Per Capita NIHB Expenditures by Region
2016/17
The national per capita expenditure for all benefits in 2016/17 was $1,388. Manitoba had the highest per capita cost in 2016/17 at $1,910. The Northern Region followed with a per capita cost of $1,594. The higher than average per capita cost for these regions is partly attributable to high medical transportation costs due to the large number of First Nations and Inuit clients living in remote or fly-in only northern communities. In contrast, the Atlantic Region had the lowest per capita cost of $851, due to the comparatively low medical transportation expenditures in the region.
Figure 3.9: Per Capita NIHB Expenditures by Region 16/17

Source: FIRMS and SVS adapted by by Business Support, Audit and Negotiations Division
Text Equivalent
| Region | Per Capita |
|---|---|
| Atlantic | $851 |
| Quebec | $1,295 |
| Ontario | $1,118 |
| Manitoba | $1,910 |
| Saskatchewan | $1,479 |
| Alberta | $1,512 |
| North | $1,594 |
| National | $1,388 |
Section 4: NIHB Pharmacy Expenditure and Utilization Data
The NIHB Program covers a comprehensive range of prescription drugs and over-the-counter medications listed on the NIHB Drug Benefit List (DBL). Coverage of pharmacy benefits and services are based on professional judgment, consistent with current best practices of health services delivery and evidence-based standards of care, with particular emphasis on client safety, intended to contribute to better health outcomes in a fair, equitable and cost-effective manner, while recognizing the unique health needs of First Nations and Inuit clients. Policies to achieve this objective have and will continue to be adopted by the NIHB Program.
In addition, a limited but comprehensive range of medical supplies and equipment (MS&E) items are covered by the Program. Like prescription and over-the-counter medications, MS&E benefits are evidence-based and covered in accordance with Program policies. Clients must obtain a prescription from a prescriber that is recognized by the NIHB Program for MS&E items, and have the prescription filled at an approved provider. Items covered under the MS&E benefit include:
- Audiology benefits, such as hearing aids and repairs;
- Medical equipment, such as wheelchairs and walkers;
- Medical supplies, such as bandages and dressings;
- Orthotics and custom footwear;
- Pressure garments;
- Prosthetics;
- Oxygen supplies and equipment; and
- Respiratory supplies and equipment.
In 2016/17, the NIHB Program paid for pharmacy and MS&E claims made by a total of 523,386 First Nations and Inuit clients. The total expenditure for these claims was $494.5 million or 41.0% of total NIHB expenditures. Of all the NIHB Program benefits, the pharmacy benefit accounts for the largest share of expenditures and is the benefit most utilized by clients.
Figure 4.1: Distribution of NIHB Pharmacy and MS&E Expenditures ($ Millions)
2016/17
In 2016/17, NIHB Pharmacy and MS&E benefits totalled $494.5 million or 41.0% of total NIHB expenditures.
Figure 4.1 illustrates the components of pharmacy and MS&E expenditures under the NIHB Program. The cost of prescription drugs paid through the Health Information and Claims Processing Services (HICPS) system was the largest component, accounting for $360.2 million or 72.8% of all NIHB Pharmacy expenditures, followed by over-the-counter (OTC) drugs and controlled access drugs (CAD) which totalled $70.4 million or 14.2%. Medical supplies and equipment (MS&E) items paid through HICPS was the third largest component in the pharmacy benefit at $36.1 million or 7.3%.
Drugs and MS&E (Regional), at $2.0 million or 0.4%, refers to regionally managed prescription drugs and OTC medications. This category also includes MS&E items paid through Indigenous Services Canada regional offices.
Contribution agreements, which accounted for $9.7 million or 2.0% of total pharmacy and MS&E benefit costs, are used to fund the provision of pharmacy benefits through agreements such as those with the Mohawk Council of Akwesasne in Ontario and the Bigstone Cree Nation in Alberta.
Other costs totalled $16.3 million or 3.3% in 2016/17. Included in this total are Headquarters contract and claims processing expenditures related to the HICPS system.
Figure 4.1: Distribution of NIHB Pharmacy and MS&E Expenditures ($ Millions) 2016/17
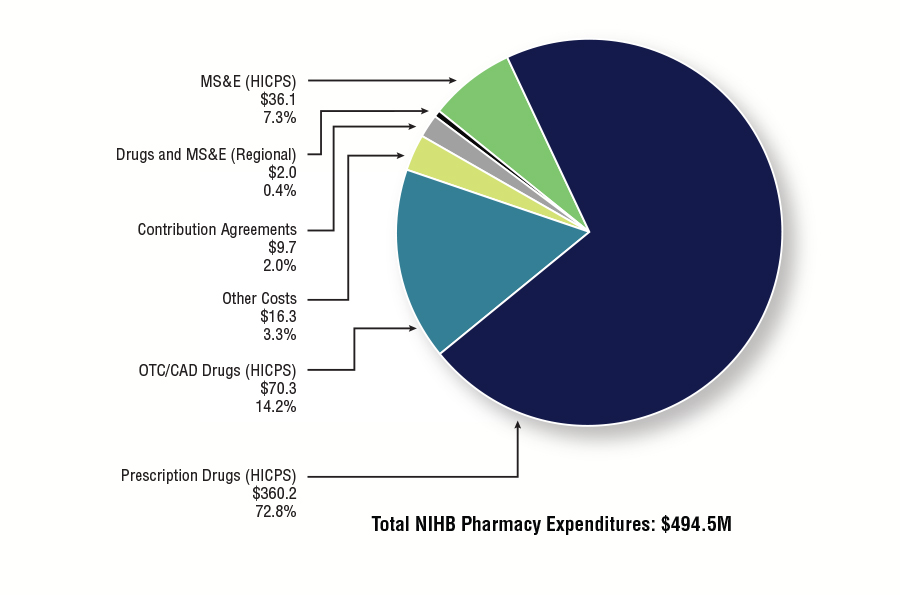
Source: FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Million $ | Proportion | |
|---|---|---|
| Prescription Drugs (HICPS) | $360.2 | 72.8% |
| OTC/CAD Drugs (HICPS) | $70.3 | 14.2% |
| Other Costs | $16.3 | 3.3% |
| Contribution Agreements | $9.7 | 2.0% |
| Drugs and MS&E (Regional) | $2.0 | 0.4% |
| MS&E (HICPS) | $36.1 | 7.3% |
| Total NIHB Pharmacy Expenditures | $494.5 | 100.0% |
Figure 4.2: Total NIHB Pharmacy Expenditures by Type and Region ($ 000's)
2016/17
Prescription drug costs paid through the HICPS system represented the largest component of total costs accounting for $360.2 million or 72.8% of all NIHB Pharmacy costs. The Saskatchewan Region had the largest proportion of these costs at 22.4%, followed by Manitoba at 20.3% and the Ontario Region at 19.6%.
The next highest component was over-the-counter (OTC) and controlled access drug (CAD) costs at $70.3 million or 14.5%. The regions of Manitoba (22.0%), Ontario (21.0%) and Saskatchewan (19.8%) had the largest proportions of these costs in 2016/17.
The third highest component was the combined medical supplies and equipment (MS&E) category at $36.1 million (7.3%). The Alberta Region (22.8%) had the highest proportion of MS&E costs in 2016/17. This was followed by the Saskatchewan Region (22.2%), the Manitoba Region (17.6%), and the Ontario Region (15.2%).
| Region | Operating | Total Operating Costs | Total Contribution Costs | Total Costs | |||||
|---|---|---|---|---|---|---|---|---|---|
| Prescription Drugs | OTC/CAD Drugs | Drugs/MS&E Regional | Medical Supplies | Medical Equipment | Other Costs | ||||
| Atlantic | $23,437 | $5,467 | $6 | $2,154 | $834 | $0 | $31,899 | $0 | $31,899 |
| Quebec | $37,151 | $8,252 | $47 | $1,275 | $720 | $0 | $47,444 | $0 | $47,444 |
| Ontario | $70,469 | $14,769 | $13 | $4,125 | $1,345 | $0 | $90,721 | $3,380 | $94,101 |
| Manitoba | $72,942 | $15,474 | $0 | $4,497 | $1,844 | $0 | $94,757 | $0 | $94,757 |
| Saskatchewan | $80,601 | $13,921 | $1,508 | $5,456 | $2,554 | $0 | $104,040 | $42 | $104,082 |
| Alberta | $53,835 | $9,171 | $23 | $5,990 | $2,227 | $0 | $71,246 | $6,023 | $77,269 |
| North | $21,603 | $3,213 | $409 | $2,074 | $977 | $0 | $28,276 | $212 | $28,488 |
| Headquarters | $0 | $0 | $0 | $0 | $0 | $16,302 | $16,302 | $0 | $16,302 |
| Total | $360,195 | $70,294 | $2,006 | $25,570 | $10,500 | $16,302 | $484,867 | $9,657 | $494,524 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | |||||||||
Figure 4.3: Annual NIHB Pharmacy Expenditures
2012/13 to 2016/17
NIHB Pharmacy expenditures increased by 8.3% during fiscal year 2016/17. Over the past five years, growth in pharmacy expenditures has ranged from a high of 8.3% in 2016/17 to a low of -10.1% in 2013/14. If expenditures for FNHA eligible clients are excluded from 2012/13 and 2013/14 total NIHB expenditures, then the growth rate for 2013/14 would have been 1.5%.
The five year annualized growth rate for NIHB Pharmacy expenditures is 1.5%. Growth has been low and steady over the past five years. Reasons for this stability include the introduction of lower cost generic drugs as they become available on the market, optimizing drug utilization, policy changes designed to promote NIHB Program sustainability, such as the implementation of the NIHB Short-Term Dispensing Policy in 2008/09, and changes in generic pricing policies in key provinces (Quebec, Ontario, Saskatchewan and British Columbia).
Figure 4.3.1: NIHB Pharmacy Expenditures and Annual Percentage Change
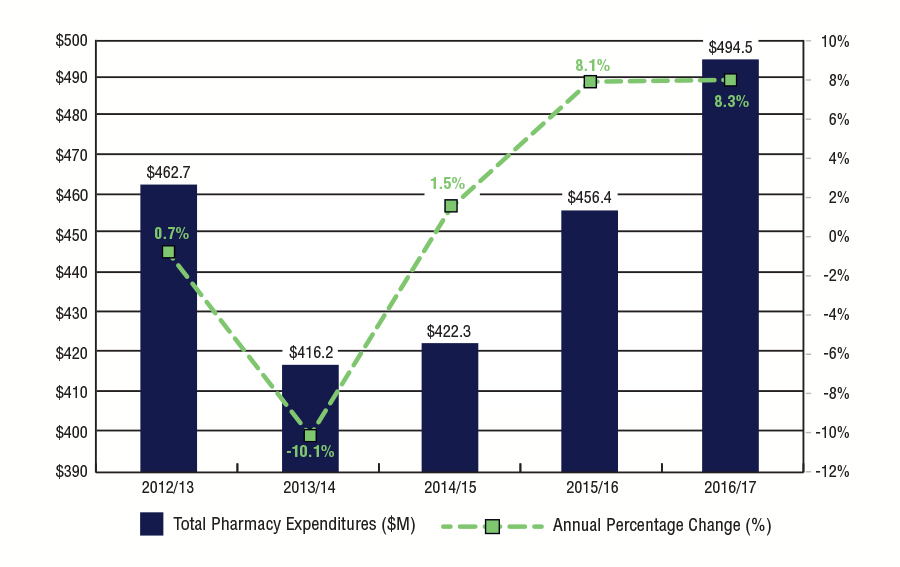
Source: FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Year | Total Pharmacy Expenditures ($M) | Annual Percentage Change (%) |
|---|---|---|
| 2012/13 | $462.7 | 0.7% |
| 2013/14 | $416.2 | -10.1% |
| 2014/15 | $422.3 | 1.5% |
| 2015/16 | $456.4 | 8.1% |
| 2016/17 | $494.5 | 8.3% |
| Region | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|
| Atlantic | $29,979 | $27,517 | $28,398 | $30,064 | $31,899 |
| Quebec | $40,393 | $40,825 | $42,581 | $44,206 | $47,444 |
| Ontario | $77,131 | $78,510 | $81,982 | $88,872 | $94,101 |
| Manitoba | $80,676 | $77,034 | $81,059 | $87,997 | $94,757 |
| Saskatchewan | $74,646 | $78,546 | $83,361 | $91,170 | $104,082 |
| Alberta | $60,584 | $58,777 | $64,087 | $69,992 | $77,265 |
| North | $15,749 | $16,874 | $16,678 | $16,546 | $16,302 |
| Headquarters | $462,699 | $416,165 | $422,350 | $456,430 | $494,520 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | |||||
Figure 4.4: Per Capita NIHB Pharmacy Expenditures by Region
2016/17
In 2016/17, the national per capita expenditure for NIHB Pharmacy benefits was $560. This was an increase of 6.9% from the $524 recorded in 2015/16.
The Saskatchewan Region had the highest per capita NIHB Pharmacy expenditure at $699, followed by the Quebec Region at $669.
The Northern Region had the lowest per capita expenditure at $415 followed by the Ontario Region at $454. A relatively low per capita expenditure in the North is attributed to lower than average utilization rates and also a younger population utilizing lower cost medications. (Refer to Figure 4.6)
Figure 4.4: Per Capita NIHB Pharmacy Expenditures by Region 2016/17
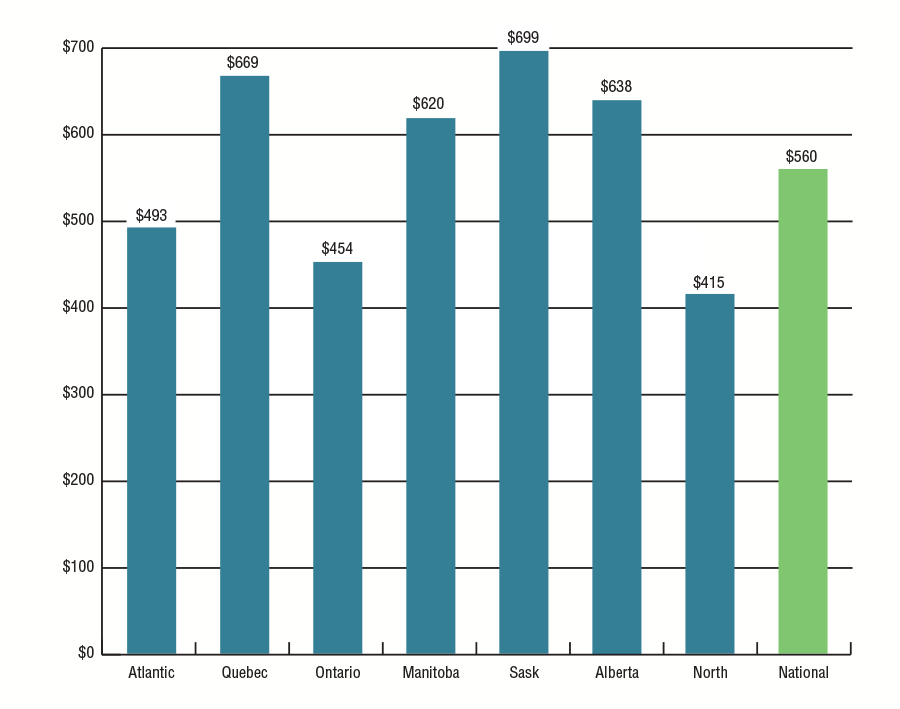
Source: FIRMS and SVS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Region | Expenditure per Capita |
|---|---|
| Atlantic | $493 |
| Quebec | $669 |
| Ontario | $454 |
| Manitoba | $620 |
| Saskatchewan | $699 |
| Alberta | $638 |
| North | $415 |
| National | $560 |
Figure 4.5: NIHB Pharmacy Operating Expenditures per Claimant by Region
2016/17
Expenditures per claimant are based on the total cost of pharmacy claims processed through the HICPS system, divided by the number of clients who submitted at least one pharmacy claim.
In 2016/17, the national average per claimant expenditure was $891, an increase of 7.0% over 2015/16.
The Quebec Region had the highest average NIHB Pharmacy operating expenditure per claimant at $1,105, followed by Saskatchewan at $989.
Figure 4.5: NIHB Pharmacy OperatingExpenditures per Claimant by Region 2016/17
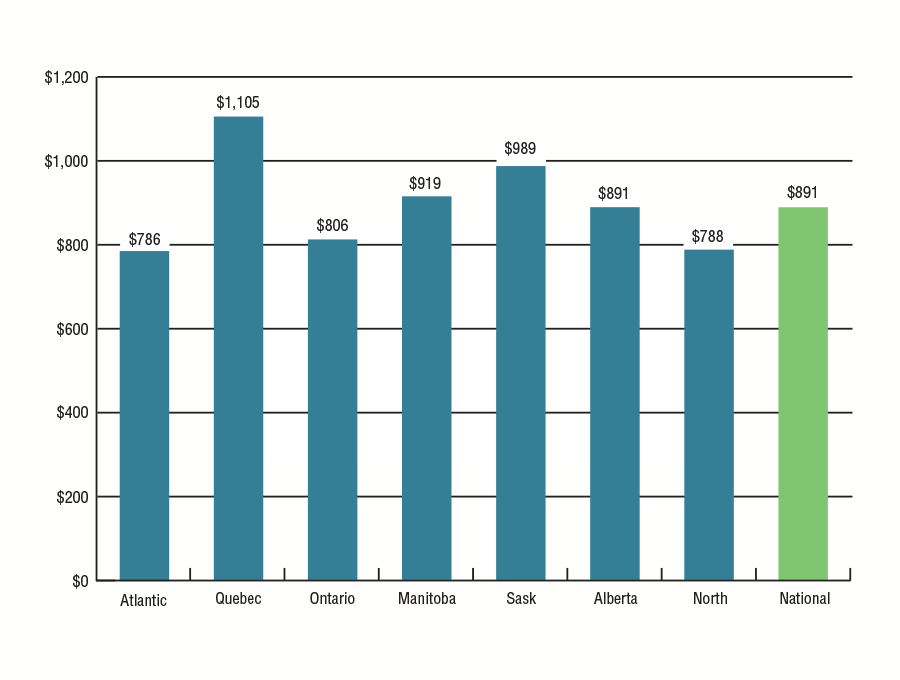
Source: HICPS and SVS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Region | Cost per Claimant |
|---|---|
| Atlantic | $786 |
| Quebec | $1,105 |
| Ontario | $806 |
| Manitoba | $919 |
| Saskatchewan | $989 |
| Alberta | $891 |
| North | $788 |
| National | $891 |
Figure 4.6: NIHB Pharmacy Utilization Rates by Region
2012/13 to 2016/17
Utilization rates represent the number of clients who received at least one pharmacy benefit paid through theHICPS system in the fiscal year, as a proportion of the total number of eligible clients.
In 2016/17, the national utilization rate was 61% for NIHB Pharmacy benefits paid through the HICPS system.
The rates understate the actual level of service as the data do not include pharmacy services provided through contribution agreements and benefits provided through community health facilities or provided completely via alternate health coverage. For example, if the Bigstone Cree Nation client population were removed from the Alberta Region's population because the HICPS system does not capture any data on services used by this population, the utilization rate for pharmacy benefits in Alberta would have been 71% in 2016/17. Similarly for the Ontario Region, if the Akwesasne client population were removed from the Ontario Region's population, the utilization rate for pharmacy benefits would have been 58%. If both the Bigstone and Akwesasne client populations were removed from the overall NIHB population, the national utilization rate for pharmacy benefits would have been 63%.
| Region | Pharmacy Utilization | ||||
|---|---|---|---|---|---|
| 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 | |
| Atlantic | 61% | 62% | 62% | 62% | 63% |
| Quebec | 59% | 59% | 60% | 60% | 60% |
| Ontario | 55% | 54% | 54% | 54% | 54% |
| Manitoba | 67% | 66% | 66% | 67% | 67% |
| Saskatchewan | 70% | 70% | 70% | 70% | 70% |
| Alberta | 66% | 66% | 66% | 66% | 66% |
| Yukon | 60% | 59% | 60% | 60% | 60% |
| N.W.T. | 53% | 53% | 54% | 54% | 55% |
| Nunavut | 46% | 46% | 47% | 46% | 47% |
| National | 62% | 61% | 61% | 61% | 61% |
| Source: HICPS and SVS adapted by Business Support, Audit and Negotiations Division | |||||
Figure 4.7: NIHB Pharmacy Claimants by Age Group, Gender and Region
2016/17
Of the 853,088 clients eligible to receive benefits under the NIHB Program, a total of 523,386 claimants, representing 61% of the NIHB client population, received at least one pharmacy item paid through the Health Information and Claims Processing Services (HICPS) system in 2016/17. Of this total, 295,340 were female (56%) and 228,046 were male (44%). This compares to the total eligible population where 51% were female and 49% were male.
The average age of pharmacy claimants was 35 years. The average age for female and male claimants was 35 and 34 years of age, respectively.
| Region | Atlantic | Quebec | Ontario | Manitoba | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age Group | Male | Female | Total | Male | Female | Total | Male | Female | Total | Male | Female | Total |
| 0-4 | 830 | 868 | 1,698 | 1,045 | 983 | 2,028 | 2,111 | 2,014 | 4,125 | 3,345 | 3,143 | 6,488 |
| 5-9 | 1,236 | 1,244 | 2,480 | 1,347 | 1,386 | 2,733 | 3,045 | 3,133 | 6,178 | 4,554 | 4,665 | 9,219 |
| 10-14 | 1,253 | 1,278 | 2,531 | 1,198 | 1,217 | 2,415 | 2,927 | 2,897 | 5,824 | 3,955 | 4,090 | 8,045 |
| 15-19 | 1,254 | 1,823 | 3,077 | 1,069 | 1,738 | 2,807 | 3,185 | 4,603 | 7,788 | 3,705 | 4,941 | 8,646 |
| 20-24 | 1,308 | 2,239 | 3,547 | 1,179 | 2,058 | 3,237 | 3,474 | 5,793 | 9,267 | 3,847 | 5,702 | 9,641 |
| 25-29 | 1,279 | 1,943 | 3,222 | 1,215 | 2,019 | 3,234 | 3,680 | 5,705 | 9,385 | 3,792 | 5,375 | 9,494 |
| 30-34 | 1,153 | 1,677 | 2,830 | 1,079 | 1,789 | 2,868 | 3,470 | 5,011 | 8,481 | 3,326 | 4,539 | 7,865 |
| 35-39 | 1,147 | 1,511 | 2,658 | 1,124 | 1,568 | 2,692 | 3,340 | 4,731 | 8,071 | 3,093 | 3,843 | 6,936 |
| 40-44 | 1,176 | 1,558 | 2,734 | 1,152 | 1,579 | 2,731 | 3,477 | 4,456 | 7,933 | 3,082 | 3,764 | 6,846 |
| 45-49 | 1,387 | 1,631 | 3,018 | 1,351 | 1,715 | 3,066 | 3,754 | 4,717 | 8,471 | 3,171 | 3,930 | 7,101 |
| 50-54 | 1,360 | 1,641 | 3,001 | 1,447 | 1,932 | 3,379 | 4,054 | 5,093 | 9,147 | 3,093 | 3,607 | 6,700 |
| 55-59 | 1,232 | 1,582 | 2,814 | 1,460 | 1,832 | 3,292 | 3,752 | 4,698 | 8,450 | 2,535 | 3,035 | 5,570 |
| 60-64 | 1,063 | 1,419 | 2,482 | 1,177 | 1,555 | 2,732 | 2,904 | 3,822 | 6,726 | 1,765 | 2,240 | 4,005 |
| 65+ | 1,924 | 2,541 | 4,465 | 2,273 | 3,411 | 5,684 | 5,081 | 7,626 | 12,707 | 2,756 | 3,749 | 6,505 |
| Total | 17,602 | 22,955 | 40,557 | 18,116 | 24,782 | 42,898 | 48,254 | 64,299 | 112,553 | 46,019 | 57,042 | 103,061 |
| Average Age | 37 | 38 | 38 | 38 | 40 | 39 | 38 | 39 | 39 | 32 | 33 | 33 |
| Source: HICPS and SVS adapted by Business Support, Audit and Negotiations Division | ||||||||||||
| Region | Saskatchewan | Alberta | North | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age Group | Male | Female | Total | Male | Female | Total | Male | Female | Total | Male | Female | Total |
| 0-4 | 3,150 | 3,052 | 6,202 | 2,640 | 2,528 | 5,168 | 1,223 | 1,134 | 2,357 | 14,623 | 13,983 | 28,606 |
| 5-9 | 4,822 | 4,953 | 9,775 | 3,860 | 3,952 | 7,812 | 1,184 | 1,117 | 2,301 | 20,196 | 20,581 | 40,777 |
| 10-14 | 4,244 | 4,573 | 8,817 | 3,284 | 3,452 | 6,736 | 945 | 936 | 1,881 | 17,929 | 18,570 | 36,499 |
| 15-19 | 3,846 | 5,377 | 9,223 | 2,984 | 3,933 | 6,917 | 918 | 1,623 | 2,541 | 17,126 | 24,272 | 41,398 |
| 20-24 | 3,847 | 6,042 | 9,889 | 3,152 | 4,424 | 7,576 | 1,083 | 2,121 | 3,204 | 18,051 | 28,755 | 46,806 |
| 25-29 | 3,951 | 5,984 | 9,935 | 3,035 | 4,212 | 7,247 | 1,082 | 2,223 | 3,305 | 18,230 | 28,129 | 46,359 |
| 30-34 | 3,470 | 4,928 | 8,398 | 2,855 | 3,677 | 6,532 | 1,043 | 1,782 | 2,825 | 16,576 | 23,699 | 40,275 |
| 35-39 | 3,218 | 4,000 | 7,218 | 2,454 | 3,206 | 5,660 | 906 | 1,519 | 2,425 | 15,444 | 20,637 | 36,081 |
| 40-44 | 2,930 | 3,799 | 6,729 | 2,258 | 2,800 | 5,058 | 858 | 1,344 | 2,202 | 15,087 | 19,521 | 34,608 |
| 45-49 | 3,032 | 3,749 | 6,781 | 2,280 | 2,679 | 4,959 | 1,178 | 1,518 | 2,696 | 16,333 | 20,185 | 36,518 |
| 50-54 | 2,773 | 3,378 | 6,151 | 2,125 | 2,626 | 4,751 | 1,081 | 1,476 | 2,557 | 16,088 | 20,028 | 36,116 |
| 55-59 | 2,292 | 2,803 | 5,095 | 1,732 | 2,185 | 3,917 | 862 | 1,239 | 2,101 | 13,969 | 17,578 | 31,547 |
| 60-64 | 1,522 | 1,957 | 3,479 | 1,188 | 1,618 | 2,806 | 650 | 904 | 1,554 | 10,338 | 13,639 | 23,977 |
| 65+ | 2,493 | 3,455 | 5,948 | 1,953 | 2,867 | 4,820 | 1,482 | 1,916 | 3,398 | 18,056 | 25,763 | 43,819 |
| Total | 45,590 | 58,050 | 103,640 | 35,800 | 44,159 | 79,959 | 14,495 | 20,852 | 35,347 | 228,046 | 295,340 | 523,386 |
| Average Age | 31 | 32 | 32 | 31 | 32 | 32 | 35 | 36 | 36 | 34 | 35 | 35 |
| Source: HICPS and SVS adapted by Business Support, Audit and Negotiations Division | ||||||||||||
Figure 4.8: Distribution of Eligible NIHB Population, Pharmacy Expenditures and Pharmacy Incidence by Age Group
2016/17
The main drivers of NIHB Pharmacy expenditures are the cost of medications, the volume of claimsFootnote 2 submitted and the professional fees associated with filling these claims. In 2016/17, 6.1% of all clients were in the 0 to 4 age group, but this group accounted for only 1.0% of all pharmacy claims made and only 1.1% of total pharmacy expenditures. In contrast, 7.8% of all eligible clients were in the 65+ age group, but accounted for 23.6 % of all pharmacy claims submitted and 17.8 % of total pharmacy expenditures.
During 2016/17, the average claimant aged 65 or more submitted 94 claims compared to 66 claims for their counterpart in the 60 to 64 age group and 6 claims for the average claimant in the 0 to 4 age group.
Figure 4.8: Distribution of Eligible NIHB Population, Pharmacy Expenditures and Pharmacy Incidence by Age Group 2016/17
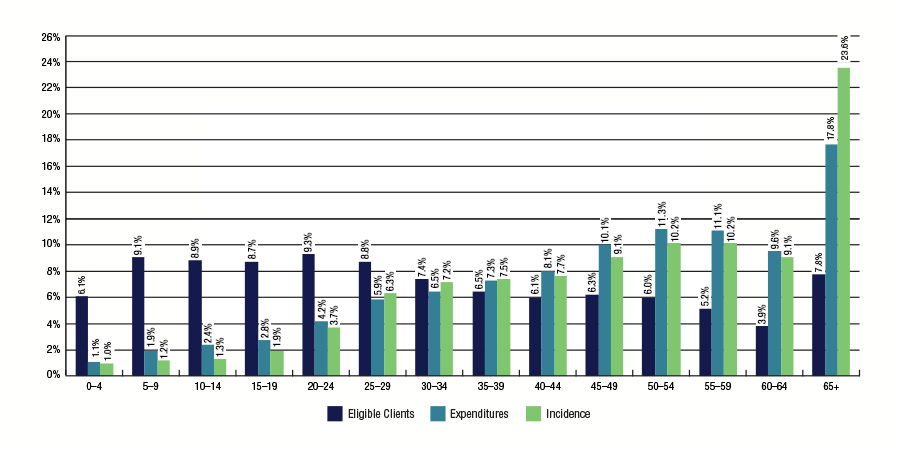
Source: HICPS and SVS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Age | Eligible Clients | Expenditures | Incidence |
|---|---|---|---|
| 0-4 | 6.1% | 1.1% | 1.0% |
| 5-9 | 9.1% | 1.9% | 1.2% |
| 10-14 | 8.9% | 2.4% | 1.3% |
| 15-19 | 8.7% | 2.8% | 1.9% |
| 20-24 | 9.3% | 4.2% | 3.7% |
| 25-29 | 8.8% | 5.9% | 6.3% |
| 30-34 | 7.4% | 6.5% | 7.2% |
| 35-39 | 6.5% | 7.3% | 7.5% |
| 40-44 | 6.1% | 8.1% | 7.7% |
| 45-49 | 6.3% | 10.1% | 9.1% |
| 50-54 | 6.0% | 11.3% | 10.2% |
| 55-59 | 5.2% | 11.1% | 10.2% |
| 60-64 | 3.9% | 9.6% | 9.1% |
| 65+ | 7.8% | 17.8% | 23.6% |
An examination of pharmacy benefit cost per NIHB claimant indicates that these expenditures vary according to age. For example, in 2016/17 the average cost per child aged 0 to 4 years was $185. The cost increased steadily for every age group, with claimants aged 35-39 having an average cost of $941, comparable to the total average claimant cost of $891. Claimants over 65 years of age had the highest cost per claimant with an average of $1,893 for all pharmaceutical services received throughout the fiscal year.
Figure 4.9: NIHB Top Ten Therapeutic Classes by Number of Claimants
2016/17
Figure 4.9 ranks the top ten therapeutic classes according to number of claimants. In 2016/17, Non-Steroidal Anti-Inflammatory Drugs (NSAID) had the highest number of distinct claimants at 200 thousand, an increase of 1.4% over 2015/16. Penicillins such as Amoxil (Amoxicillin) ranked second in number of claimants with 162 thousand followed by Opioid Agonists with 121 thousand claimants.
| Therapeutic Classification | Claimants | % Change from 2015/16 | Examples of Product in the Therapeutic Class |
|---|---|---|---|
| Non-Steroidal Anti-Inflammatory Drugs (NSAID) | 200,430 | 1.4% | Voltaren (Diclofenac) |
| Penicillins | 161,920 | 1.3% | Amoxil (Amoxicillin) |
| Opioid Agonists | 120,875 | 1.3% | Statex (Morphine Sulphate) |
| Miscellaneous Analgesics and Antipyretics | 117,887 | 4.6% | Tylenol (Acetaminophen) |
| Antidepressants | 90,378 | 7.2% | Losec (Omeprazole) |
| Proton Pump Inhibitors | 89,120 | 4.0% | Ventolin (Salbutamol) |
| Beta-Adrenergic Agonists | 86,837 | 2.4% | Effexor (Venlafaxine) |
| SMMA - Anti-inflammatory Agents | 79,769 | 3.5% | Cortate Cream (Hydrocortisone) |
| Cephalosporins | 75,534 | 2.3% | Keflex (Cephalexin) |
| Adrenals | 70,047 | 0.1% | Flovent (Fluticasone Propionate) |
| Source: HICPS adapted by Business Support, Audit and Negotiations Division | |||
Figure 4.10: NIHB Prescription Drug Claims Incidence by Pharmacologic Therapeutic Class
2016/17
Figure 4.10 demonstrates variation in claims incidence by therapeutic classification for prescription drugs.
Central nervous system agents, which include drug classes such as analgesics and sedatives, accounted for 43.3% of all prescription drug claims in 2016/17. Central nervous systems agents are used in the treatment of diverse health conditions such as arthritis, depression or epilepsy.
Cardiovascular drugs had the next highest share of prescription drug claims at 17.4% followed by hormones and synthetic substitutes, which consist primarily of oral contraceptives and insulin, at 11.4%. Cardiovascular drugs are used to treat clients with arrhythmias, hypercholesterolemia or ischemic heart disease. Hormones and synthetic substitutes are given to clients to treat conditions such as diabetes or hypothyroidism.
Figure 4.10: NIHB Prescription Drug Claims Incidence by Pharmacologic Therapeutic Class 2016/17
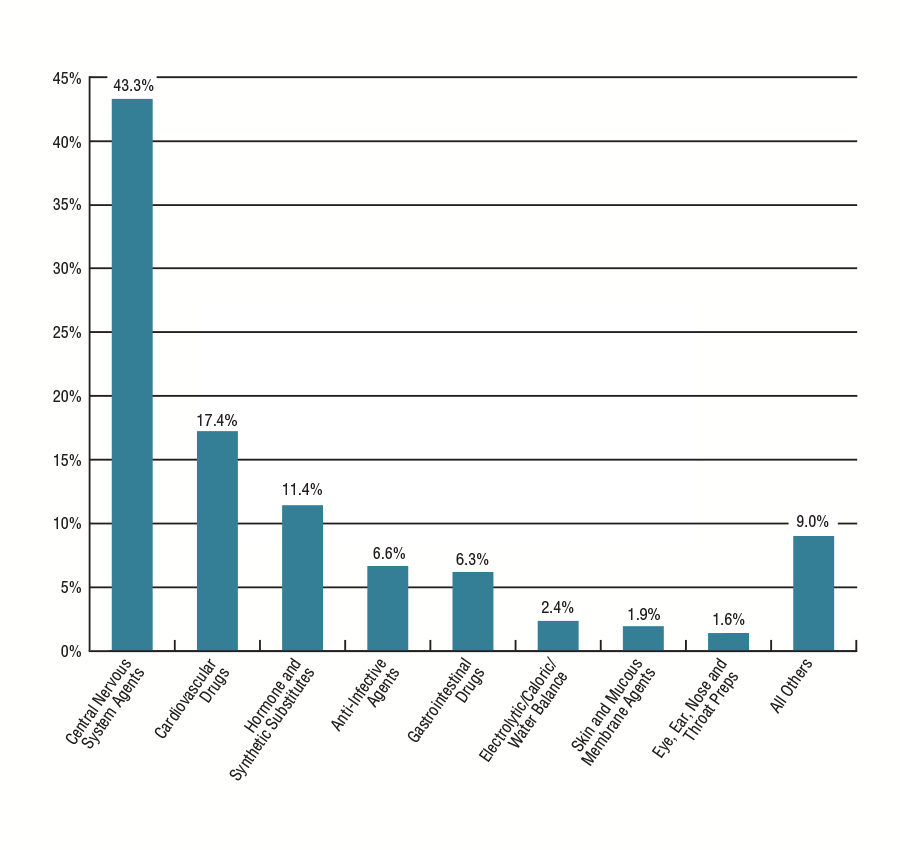
Source: HICPS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Sub-benefit | % |
|---|---|
| Central Nervous System Agents | 43.3% |
| Cardiovascular Drugs | 17.4% |
| Hormones and Synthetic Substitutes | 11.4% |
| Anti-Infective Agents | 6.6% |
| Gastrointestinal Drugs | 6.3% |
| Electrolytic/Caloric/Water Balance | 2.4% |
| Skin and Mucous Membrane Agents | 1.9% |
| Eye, Ear, Nose and Throat Preps | 1.6% |
| All Others | 9.0% |
Figure 4.11: NIHB Over-the-Counter Drugs (Including Controlled Access Drugs - CAD) Claims Incidence by Pharmacologic Therapeutic Class
2016/17
Figure 4.11 demonstrates variation in claims incidence by therapeutic classification for over-the-counter (OTC) drugs. The NIHB Program covers the cost of some OTC drugs. To be reimbursed by the NIHB Program, all OTC drugs require a prescription from a recognized health professional who has the authority to prescribe in their province or territory of practice.
OTC central nervous system agents, which are drugs used to manage pain such as headaches (e.g. acetaminophen), accounted for 25.9% of all OTC drug claims.
Vitamins are the next highest category of OTC medication at 25.1%, followed by gastrointestinal products such as antacids and laxatives, which are used to treat heartburn and constipation, at 9.3%.
Figure 4.11: NIHB Over-the-Counter Drugs (Including Controlled Access Drugs - CAD) Claims Incidence by Pharmacologic Therapeutic Class 2016/17
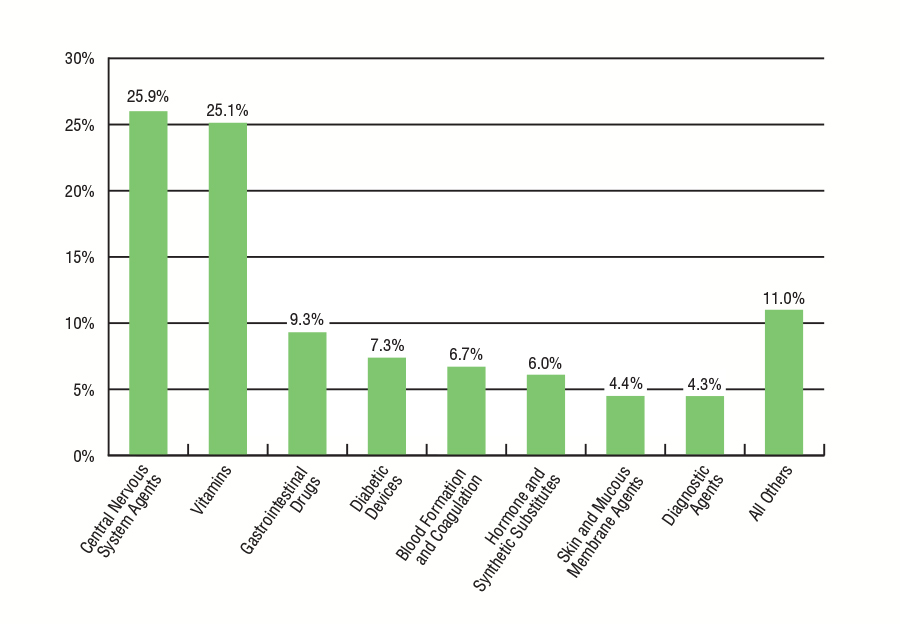
Source: HICPS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Sub-Benefit | Claims % |
|---|---|
| Central Nervous System Agents | 25.9% |
| Vitamins | 25.1% |
| Gastrointestinal Drugs | 9.3% |
| Diabetic Devices | 7.3% |
| Blood Formation and Coagulation | 6.7% |
| Hormones and Synthetic Substitutes | 6.0% |
| Skin and Mucous Membrane Agents | 4.4% |
| Diagnostic Agents | 4.3% |
| All Others | 11.0% |
Figure 4.12: Medical Supplies by Category and Claims Incidence
2016/17
Figure 4.12 demonstrates variation in medical supply claims incidence by category.
In 2016/17, incontinence supplies such as liners and pads accounted for 24.7% of all medical supply claims. Hearing aid supplies, such as batteries, represented 23.5% of all medical supply claims, followed by wound care supplies at 23.2%.
Figure 4.12: Medical Supplies by Category and Claims Incidence 2016/17
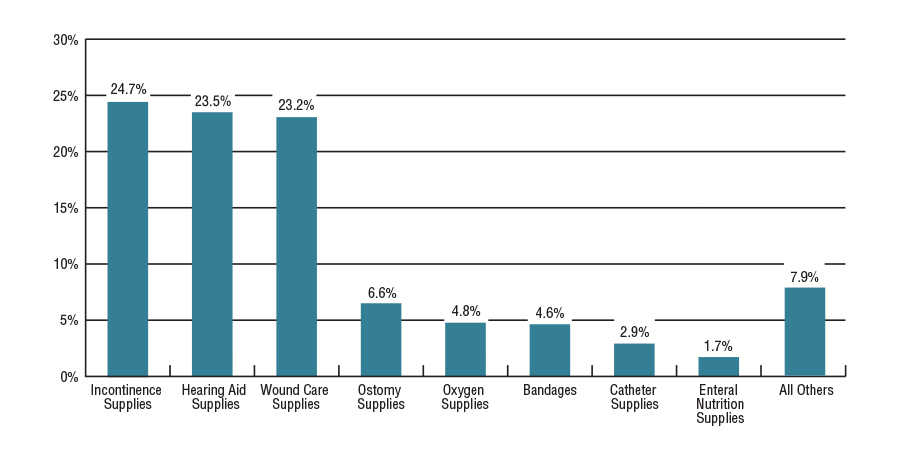
Source: HICPS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Sub-Benefit | Claims % |
|---|---|
| Incontinence Supplies | 24.7% |
| Hearing Aid Supplies | 23.5% |
| Wound Care Supplies | 23.2% |
| Ostomy Supplies | 6.6% |
| Oxygen Supplies | 4.8% |
| Bandages | 4.6% |
| Catheter Supplies | 2.9% |
| Enteral Nutrition supplies | 1.7% |
| All Others | 7.9% |
Figure 4.13: NIHB Medical Equipment by Category and Claims Incidence
2016/17
Figure 4.13 demonstrates variation in medical equipment claims incidence by category.
Claims for hearing aids accounted for 24.9% of all medical equipment claims in 2016/17. Oxygen equipment was the next highest at 24.1%, followed by limb orthoses at 9.2% and walking aids at 8.6%.
The most significant increase in the proportion of total medical equipment claims over the fiscal year 2015/16 was in hearing aids which increased by 3.0 percentage points.
Figure 4.13: NIHB Medical Equipment by Category and Claims Incidence 2016/17
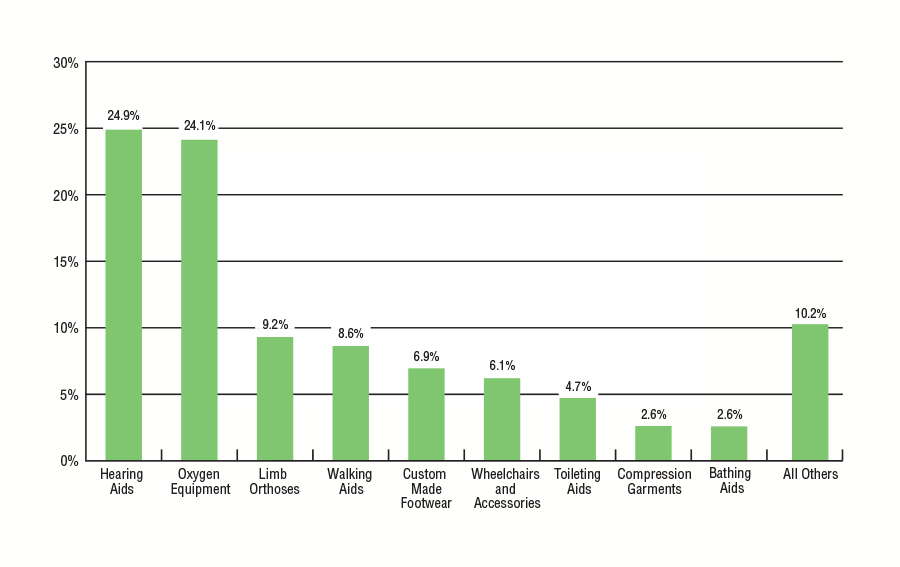
Source: HICPS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Sub-Benefit | Claims % |
|---|---|
| Hearing Aids | 24.9% |
| Oxygen Equipment | 24.1% |
| Limb Orthoses | 9.2% |
| Walking Aids | 8.6% |
| Custom Made Footwear | 6.9% |
| Wheelchairs and Accessories | 6.1% |
| Toileting Aids | 4.7% |
| Compression Garments | 2.6% |
| Bathing Aids | 2.6% |
| All Others | 10.2% |
Section 5: NIHB Dental Expenditure and Utilization Data
The NIHB Program recognizes the importance of good oral health in contributing to the overall health of First Nations and Inuit clients, and covers a broad range of dental services in an effort to address the unique oral health needs of this client population.
In 2016/17, a total of 306,705 First Nations and Inuit clients accessed dental benefits through the NIHB Program, based on claims paid through the HICPS system. The total expenditure for dental benefit claims was $235.8 million or 19.5% of total NIHB expenditures. The dental benefit accounts for the third largest Program expenditure.
Coverage for NIHB Dental benefits is based on scientific evidence and current standards of care, and takes into consideration the client's current oral health status and treatment history and accumulated scientific research. Dental services must be provided by a licensed dental professional, such as a dentist, dental specialist, or denturist. Some dental services require predetermination prior to the initiation of treatment. Predetermination is a review that determines if the proposed dental service is covered under the Program's policies and criteria, as described in the NIHB Dental Benefits Guide.
The range of dental services covered by the NIHB Program, includes:
- Diagnostic services such as examinations and radiographs;
- Preventive services such as scaling, polishing, fluorides and sealants;
- Restorative services such as fillings and crowns;
- Endodontic services such as root canal treatments;
- Periodontal services such as deep scaling;
- Removable prosthodontic services such as dentures;
- Oral surgery services such as extractions;
- Orthodontic services to correct significant irregularities in teeth and jaws; and
- Adjunctive services such as general anaesthesia and sedation.
Figure 5.1: Distribution of NIHB Dental Expenditures ($ Millions)
2016/17
NIHB Dental expenditures totalled $235.8 million in 2016/17. Figure 5.1 illustrates the distinct components of dental expenditures under the NIHB Program. Fee-for-service dental costs paid through the Health Information and Claims Processing Services (HICPS) system represented the largest expenditure component, accounting for $212.2 million or 90.0% of all NIHB Dental costs.
The next highest component was contribution agreements, which accounted for $12.6 million or 5.3% of total dental expenditures. Contribution allocations were used to fund the provision of dental benefits through agreements such as those with the Mohawk Council of Akwesasne in Ontario and the Bigstone Cree Nation in Alberta.
Expenditures for contract dentists providing services to clients in remote communities totalled $8.1 million or 3.4% of total costs.
Other costs totalled $2.9 million or 1.2% in 2016/17. The majority of these costs are related to benefit claims processing through the HICPS system.
Figure 5.1: Distribution of NIHB Dental Expenditures ($ Millions) 2016/17
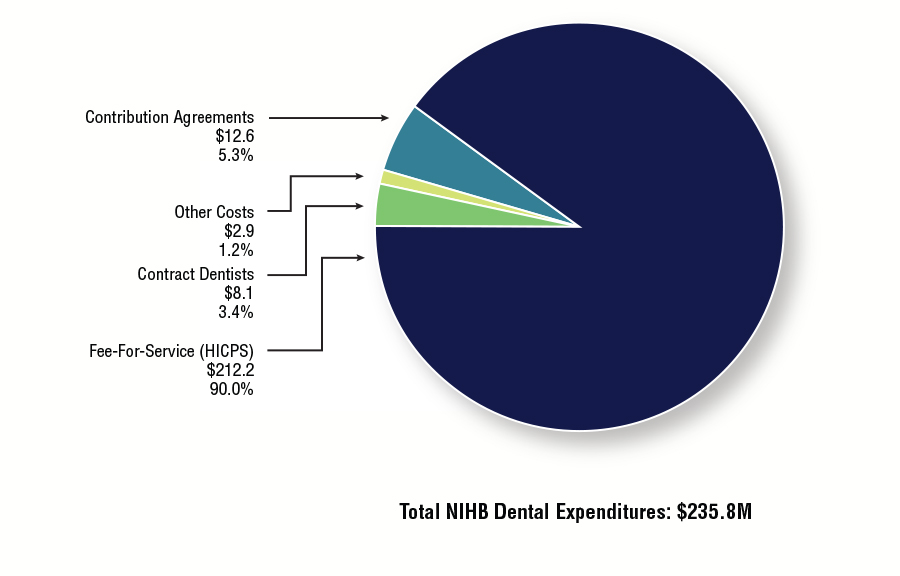
Source: FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Million $ | Proportion | |
|---|---|---|
| Fee-For-Service (HICPS) | $212.2 | 90.0% |
| Contribution Agreements | $12.6 | 5.3% |
| Other Costs | $2.9 | 1.2% |
| Contract Dentists | $8.1 | 3.4% |
| Total NIHB Dental Expenditures | $235.8 | 100.0% |
Figure 5.2: Total NIHB Dental Expenditures by Type and Region ($ 000's)
2016/17
NIHB Dental expenditures totalled $235.8 million in 2016/17. The regions of Ontario (22.1%), Saskatchewan (20.1%), Alberta (18.8%) and Manitoba (17.0%) had the largest proportion of overall dental costs. The Ontario Region had the highest total dental expenditure at $52.1 million and the Atlantic Region had the lowest total dental expenditure at $9.6 million.
| Region | Operating | Total Operating Costs | Total Contribution Costs | Total Costs | ||
|---|---|---|---|---|---|---|
| Fee-For-Service | Contract Dentists | Other Costs | ||||
| Atlantic | $9,593 | $0 | $0 | $9,593 | - | $9,593 |
| Quebec | $17,456 | $0 | $0 | $17,456 | $113 | $17,569 |
| Ontario | $43,094 | $2,614 | $46 | $45,754 | $6,350 | $52,105 |
| Manitoba | $34,887 | $5,046 | $0 | $39,933 | $53 | $39,986 |
| Saskatchewan | $43,727 | $0 | $0 | $43,727 | $3,593 | $47,321 |
| Alberta | $41,983 | $41 | $0 | $42,025 | $2,290 | $44,315 |
| North | $21,406 | $353 | $0 | $21,759 | $207 | $21,966 |
| Headquarters | - | - | $2,877 | $2,877 | - | $2,877 |
| Total | $212,248 | $8,055 | $2,923 | $223,226 | $12,605 | $235,831 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | ||||||
Figure 5.3: Annual NIHB Dental Expenditures
2012/13 to 2016/17
NIHB Dental expenditures increased by 8.6% during fiscal year 2016/17. The decrease in overall NIHB Dental expenditures recorded in fiscal years 2013/14 and 2014/15 can be attributed to the transfer of eligible First Nation clients residing in British Columbia to the First Nations Health Authority (FNHA). If expenditures for FNHA eligible clients are excluded from 2012/13 and 2013/14 total NIHB expenditures, then the dental expenditure growth rate for 2013/14 would have been 3.8%.
Over the last five years, annual growth rates for NIHB Dental expenditures have ranged from a high of 8.6% in 2016/17 to a low of -7.0% in 2013/14.
Figure 5.3.1: NIHB Dental Expenditures and Annual Percentage Change
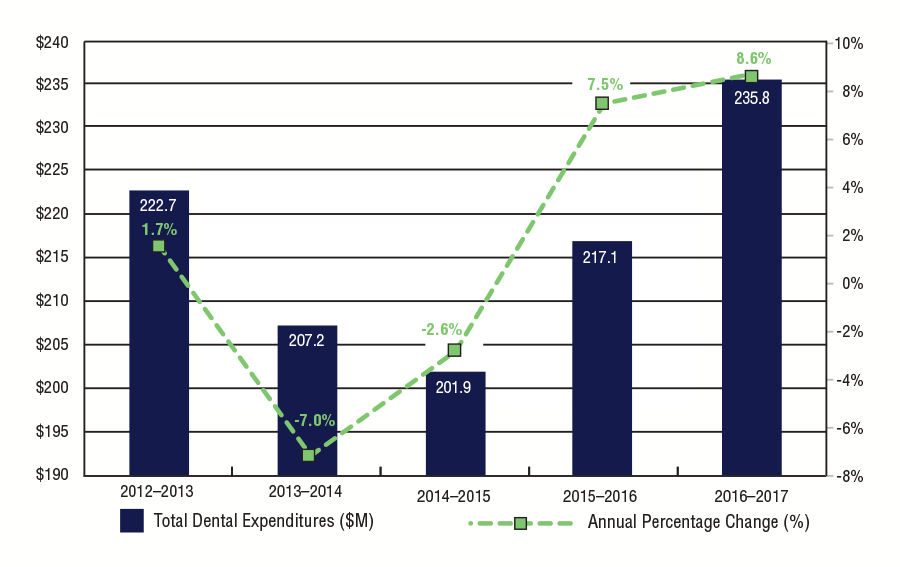
Source: NIHB Dental Expenditures and Annual Percentage Change
Text Equivalent
| Year | Total Dental Expenditures ($M) | Annual Percentage Change (%) |
|---|---|---|
| 2012/13 | $222.7 | 1.7% |
| 2013/14 | $207.2 | -7.0% |
| 2014/15 | $201.9 | -2.6% |
| 2015/16 | $217.1 | 7.5% |
| 2016/17 | $235.8 | 8.6% |
| Region | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|
| Atlantic | $9,660 | $8,609 | $8,238 | $8,846 | $9,593 |
| Quebec | $15,239 | $15,216 | $15,799 | $16,641 | $17,569 |
| Ontario | $42,259 | $43,972 | $46,759 | $49,903 | $52,105 |
| Manitoba | $30,734 | $33,649 | $33,527 | $36,764 | $39,986 |
| Saskatchewan | $36,219 | $36,399 | $37,679 | $41,028 | $47,321 |
| Alberta | $34,501 | $34,928 | $35,974 | $39,753 | $44,315 |
| North | $19,773 | $20,415 | $20,413 | $20,936 | $21,966 |
| Headquarters | $2,779 | $2,978 | $2,943 | $2,920 | $2,877 |
| Total | $222,706 | $207,179 | $201,886 | $217,109 | $235,831 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | |||||
Figure 5.4: Per Capita NIHB Dental Expenditures by Region
2016/17
In 2016/17, the national per capita NIHB Dental expenditure was $273, an increase of 7.0% from $255 recorded in 2015/16.
The Alberta Region had the highest per capita dental expenditure at $366, followed closely by the Northern Region at $328 and Saskatchewan Region at $317. The Atlantic Region had the lowest per capita dental cost at $148 per eligible client. The lower per capita cost in the Atlantic Region can be partly attributed to an increase in the eligible client population in this region as a result of the registration of 24,745 Qalipu Mi'kmaq First Nations clients. A large number of these clients have alternative dental coverage, so the lower level of dental benefit utilization for these new clients has impacted the dental per capita cost for the Atlantic Region as a whole.
Per capita values reflect NIHB Dental expenditures only, and do not include additional dental services that may be provided to First Nations and Inuit populations through other Department of Indigenous Services Canada programs or through transfers and other arrangements.
Figure 5.4: Per Capita NIHB Dental Expenditures by Region 2016/17
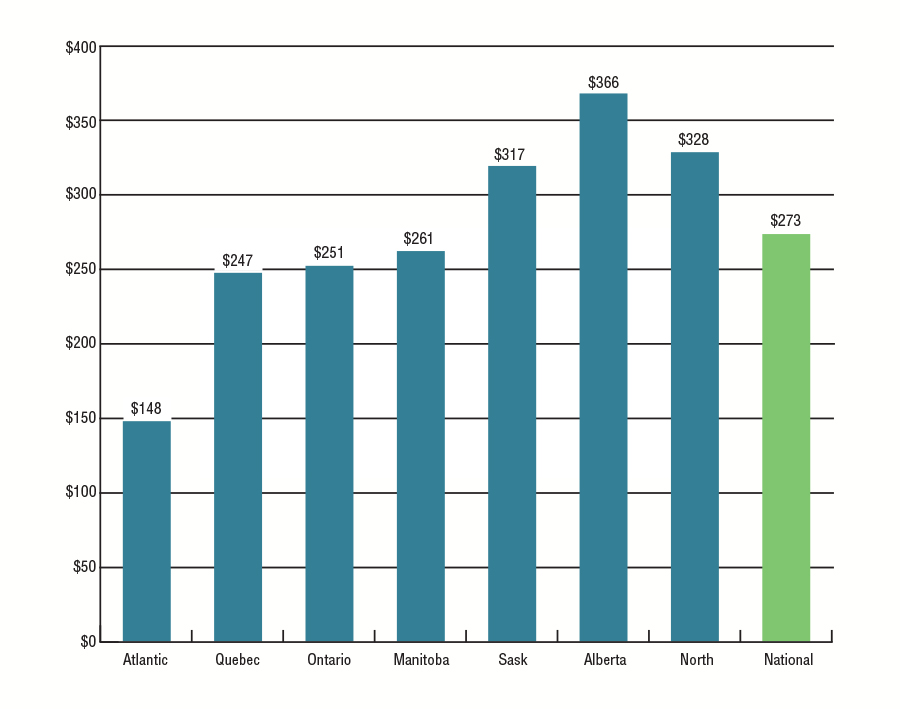
Source: SVS and FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Region | Per Capita Expenditures |
|---|---|
| Atlantic | $148 |
| Quebec | $247 |
| Ontario | $251 |
| Manitoba | $261 |
| Saskatchewan | $317 |
| Alberta | $366 |
| North | $328 |
| National | $273 |
Figure 5.5: NIHB Dental Fee-For-Service Expenditures per Claimant by Region
2016/17
In 2016/17, the national NIHB Dental expenditure per claimant (i.e. eligible clients who received at least one dental benefit) was $692. This represents an increase of 6.2% over the $652 recorded in 2015/16.
The Alberta Region had the highest dental expenditure per claimant at $853 followed by the Northern Region at $802, an increase of 7.4% and 4.6% respectively from $794 and $767 in the previous year.
Figure 5.5: NIHB Dental Fee-For-Service Expenditures per Claimant by Region 2016/17
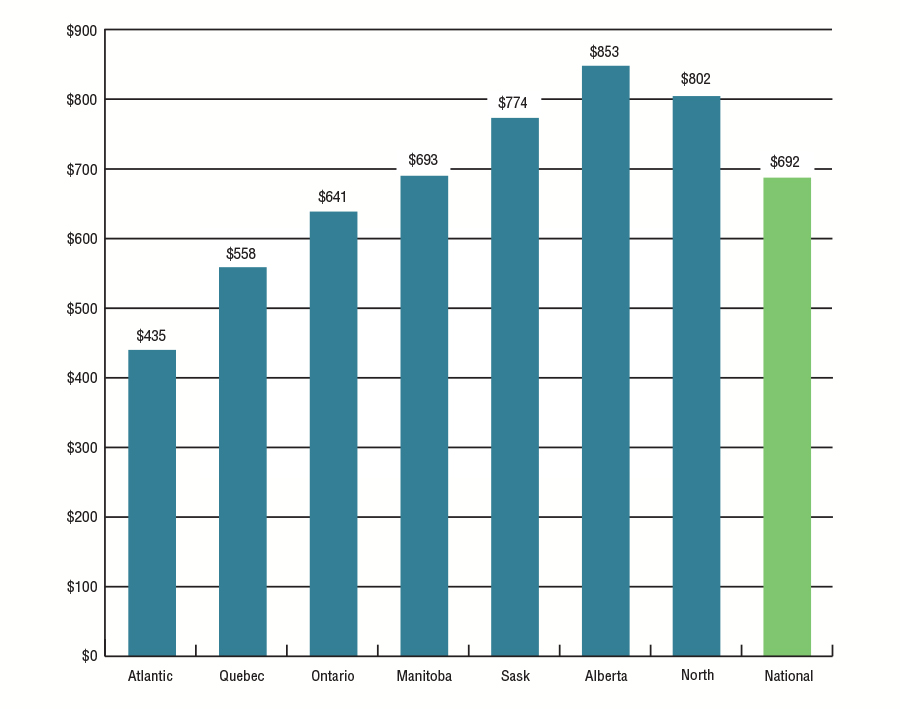
Source: FIRMS and HICPS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Region | Per Claimant |
|---|---|
| Atlantic | $435 |
| Quebec | $558 |
| Ontario | $641 |
| Manitoba | $693 |
| Saskatchewan | $774 |
| Alberta | $853 |
| North | $802 |
| National | $692 |
Figure 5.6: NIHB Dental Utilization Rates by Region
2012/13 to 2016/17
Utilization rates reflect the number of clients who, during the fiscal year, received at least one dental service paid through the HICPS system as a proportion of the total number of eligible clients.
In 2016/17, the national utilization rate for dental benefits paid through the HICPS system was 36%, consistent with the previous four fiscal years. National NIHB Dental utilization rates have remained stable over the past five years.
Dental utilization rates vary across the regions with the highest dental utilization rate found in the Quebec Region (44%). The lowest dental utilization rate was in the Ontario Region (32%). It should be noted that the dental utilization rates understate the actual level of service, as this data does not include:
- Department of Indigenous Services Canada dental clinics (except in the Yukon);
- Contract dental services provided in some regions;
- Services provided by Department of Indigenous Services Canada Dental Therapists or other FNIHB dental programs such as the Children's Oral Health Initiative (COHI); and
- Dental services provided through contribution agreements. For example, HICPS data does not capture any services utilized by the Bigstone Cree Nation. If this client population was removed from the Alberta Region's population, the utilization rate for dental benefits for Alberta would have been 43% in 2016/17. The same scenario would apply for the Ontario Region. If the Akwesasne client population in Ontario were to be removed, the utilization rate for dental benefits in Ontario would have been 35%. If both the Bigstone and Akwesasne client populations were removed from the overall NIHB population, the national utilization rate for dental benefits would have been 37%.
Over the two year period between 2015/16 and 2016/17, 412,479 distinct clients received NIHB Dental services resulting in an overall 48% utilization rate over this period.
| Region | Dental Utilization | NIHB Dental Utilization Last Two Years 2015/17 | ||||
|---|---|---|---|---|---|---|
| 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 | ||
| Atlantic | 34% | 34% | 33% | 34% | 34% | 44% |
| Quebec | 44% | 45% | 45% | 45% | 44% | 56% |
| Ontario | 32% | 32% | 32% | 32% | 32% | 42% |
| Manitoba | 31% | 32% | 32% | 32% | 33% | 46% |
| Saskatchewan | 36% | 36% | 36% | 36% | 38% | 53% |
| Alberta | 39% | 41% | 39% | 40% | 41% | 55% |
| Yukon | 37% | 39% | 37% | 36% | 36% | 50% |
| N.W.T. | 41% | 43% | 41% | 40% | 41% | 55% |
| Nunavut | 42% | 43% | 42% | 40% | 38% | 55% |
| National | 36% | 36% | 35% | 35% | 36% | 48% |
| Source: HICPS and SVS adapted by Business Support, Audit and Negotiations Division | ||||||
Figure 5.7: NIHB Dental Claimants by Age Group, Gender and Region
2016/17
Of the 853,088 clients eligible to receive dental benefits through the NIHB Program, 306,705 (36%) claimants received at least one dental procedure paid through the HICPS system in 2016/17.
Of this total, 171,841 were female (56%) and 134,864 were male (44%), compared to the total eligible NIHB population where 51% were female and 49% were male.
The average age of dental claimants was 31 years, indicating clients tend to access dental services at a slightly younger age compared to pharmacy services (35 years of age). The average age for female and male claimants was 32 and 30 years of age respectively.
Approximately 37% of all dental claimants were under 20 years of age. Forty percent of male claimants were in this age group compared to 34% of female claimants. Approximately 5% of all claimants were seniors (ages 65 and over) in 2016/17.
| Region | Atlantic | Quebec | Ontario | Manitoba | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age Group | Male | Female | Total | Male | Female | Total | Male | Female | Total | Male | Female | Total |
| 0-4 | 113 | 150 | 263 | 353 | 383 | 736 | 937 | 1,054 | 1,991 | 1,397 | 1,396 | 2,793 |
| 5-9 | 629 | 671 | 1,300 | 1,641 | 1,624 | 3,265 | 3,348 | 3,368 | 6,716 | 3,085 | 3,227 | 6,312 |
| 10-14 | 836 | 872 | 1,708 | 1,676 | 1,527 | 3,203 | 3,361 | 3,334 | 6,695 | 2,902 | 3,199 | 6,101 |
| 15-19 | 1,015 | 1,201 | 2,216 | 1,199 | 1,430 | 2,629 | 2,913 | 3,206 | 6,119 | 2,353 | 2,880 | 5,233 |
| 20-24 | 880 | 1,185 | 2,065 | 1,116 | 1,391 | 2,507 | 2,337 | 3,070 | 5,407 | 1,928 | 2,771 | 4,699 |
| 25-29 | 806 | 1,105 | 1,911 | 1,022 | 1,364 | 2,386 | 2,180 | 3,206 | 5,386 | 1,857 | 2,723 | 4,580 |
| 30-34 | 751 | 932 | 1,683 | 855 | 1,203 | 2,058 | 1,924 | 2,687 | 4,611 | 1,443 | 2,009 | 3,452 |
| 35-39 | 645 | 835 | 1,480 | 835 | 1,135 | 1,970 | 1,753 | 2,457 | 4,210 | 1,286 | 1,794 | 3,080 |
| 40-44 | 630 | 899 | 1,529 | 877 | 1,149 | 2,026 | 1,767 | 2,279 | 4,046 | 1,274 | 1,697 | 2,971 |
| 45-49 | 725 | 935 | 1,660 | 943 | 1,180 | 2,123 | 1,818 | 2,487 | 4,305 | 1,233 | 1,676 | 2,909 |
| 50-54 | 689 | 887 | 1,576 | 965 | 1,272 | 2,237 | 1,908 | 2,736 | 4,644 | 1,213 | 1,524 | 2,737 |
| 55-59 | 617 | 868 | 1,485 | 897 | 1,189 | 2,086 | 1,750 | 2,469 | 4,219 | 929 | 1,238 | 2,167 |
| 60-64 | 521 | 810 | 1,331 | 644 | 907 | 1,551 | 1,301 | 2,053 | 3,354 | 602 | 882 | 1,484 |
| 65+ | 784 | 1,042 | 1,826 | 1,036 | 1,494 | 2,530 | 2,105 | 3,445 | 5,550 | 714 | 1,120 | 1,834 |
| Total | 9,641 | 12,392 | 22,033 | 14,059 | 17,248 | 31,307 | 29,402 | 37,851 | 67,253 | 22,216 | 28,136 | 50,352 |
| Average Age | 36 | 37 | 37 | 33 | 36 | 35 | 33 | 36 | 34 | 28 | 29 | 29 |
| Source: HICPS adapted by Business Support, Audit and Negotiations Division | ||||||||||||
| Region | Saskatchewan | Alberta | North | TOTAL | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age Group | Male | Female | Total | Male | Female | Total | Male | Female | Total | Male | Female | Total |
| 0-4 | 1,311 | 1,467 | 2,778 | 1,381 | 1,389 | 2,770 | 861 | 794 | 1,655 | 6,446 | 6,732 | 13,178 |
| 5-9 | 3,646 | 3,784 | 7,430 | 3,688 | 3,678 | 7,366 | 1,305 | 1,379 | 2,684 | 17,521 | 17,902 | 35,423 |
| 10-14 | 3,341 | 3,782 | 7,123 | 3,101 | 3,424 | 6,525 | 1,204 | 1,454 | 2,658 | 16,582 | 17,752 | 34,334 |
| 15-19 | 2,492 | 3,219 | 5,711 | 2,376 | 2,840 | 5,216 | 1,091 | 1,465 | 2,556 | 13,593 | 16,401 | 29,994 |
| 20-24 | 2,013 | 3,225 | 5,238 | 1,795 | 2,466 | 4,261 | 1,133 | 1,661 | 2,794 | 11,326 | 15,921 | 27,247 |
| 25-29 | 2,141 | 3,227 | 5,368 | 1,658 | 2,400 | 4,058 | 1,101 | 1,621 | 2,722 | 10,895 | 15,848 | 26,743 |
| 30-34 | 1,700 | 2,556 | 4,256 | 1,499 | 2,090 | 3,589 | 870 | 1,301 | 2,171 | 9,166 | 12,950 | 22,116 |
| 35-39 | 1,578 | 2,039 | 3,617 | 1,269 | 1,767 | 3,036 | 743 | 973 | 1,716 | 8,194 | 11,145 | 19,339 |
| 40-44 | 1,373 | 1,912 | 3,285 | 1,088 | 1,570 | 2,658 | 640 | 869 | 1,509 | 7,732 | 10,495 | 18,227 |
| 45-49 | 1,519 | 1,931 | 3,450 | 1,112 | 1,468 | 2,580 | 752 | 939 | 1,691 | 8,206 | 10,756 | 18,962 |
| 50-54 | 1,257 | 1,629 | 2,886 | 1,018 | 1,435 | 2,453 | 622 | 821 | 1,443 | 7,751 | 10,453 | 18,204 |
| 55-59 | 1,002 | 1,277 | 2,279 | 760 | 1,122 | 1,882 | 441 | 650 | 1,091 | 6,449 | 8,909 | 15,358 |
| 60-64 | 551 | 777 | 1,328 | 532 | 771 | 1,303 | 326 | 457 | 783 | 4,510 | 6,715 | 11,225 |
| 65+ | 689 | 1,063 | 1,752 | 601 | 936 | 1,537 | 521 | 686 | 1,207 | 6,493 | 9,862 | 16,355 |
| Total | 24,613 | 31,888 | 56,501 | 21,878 | 27,356 | 49,234 | 11,610 | 15,070 | 26,680 | 134,864 | 171,841 | 306,705 |
| Average Age | 27 | 29 | 28 | 26 | 28 | 27 | 29 | 30 | 30 | 30 | 32 | 31 |
| Source: HICPS adapted by Business Support, Audit and Negotiations Division | ||||||||||||
Figure 5.8: NIHB Fee-for-Service Dental Expenditures by Sub-Benefit
2016/17
First Nations and Inuit experience a higher rate of dental disease such as periodontal disease and caries compared to other Canadians. Poor oral health can contribute to a greater incidence and severity of other medical conditions such as diabetes, respiratory illnesses and cardiovascular diseases. The broad range of dental services covered by the NIHB Program provides the opportunity to ensure that proper oral care required for overall good health is available to First Nations and Inuit clients. In 2016/17, through the NIHB Program's Dental Benefit, the oral health needs of approximately 202,000 clients who required intraoral radiograph services, 189,000 clients who received scaling procedures, and 142,000 clients who required restoration treatments were addressed.
In 2016/17, expenditures for Restorative Services (crowns, fillings, etc.) were the highest of all dental sub-benefit categories at $94.9 million. Diagnostic Services (examinations, x-rays, etc.) at $27.9 million and Preventative Services (scaling, sealants, etc.) at $26.3 million were the next highest sub-benefit categories. Rounding out the top 5 was Oral Surgery (extractions, etc.) at $24.3 million and Endodontic Services (root canal treatments, etc.) at $13.3 million.
In 2016/17, the three largest dental procedures by expenditure were Composite Restorations ($80.1 million), Scaling ($20.2 million) and Extractions ($17.0 million).
| Dental Sub-Benefit | 2015/16 | 2016/17 | % Change from 2015/16 |
|---|---|---|---|
| Restorative Services | $87.0 | $94.9 | 9.2% |
| Diagnostic Services | $24.4 | $27.9 | 14.7% |
| Preventative Services | $24.5 | $26.3 | 7.1% |
| Oral Surgery | $22.6 | $24.3 | 7.5% |
| Endodontic Services | $11.3 | $13.3 | 17.8% |
| Source: HICPS adapted by Business Support, Audit and Negotiations Division | |||
| Dental Procedure | 2015/16 | 2016/17 | % Change from 2015/16 |
|---|---|---|---|
| Composite Restorations | $72.6 | $80.1 | 10.3% |
| Scaling | $18.8 | $20.2 | 7.7% |
| Extractions | $16.0 | $17.0 | 6.1% |
| Root Canal Therapy | $9.3 | $11.3 | 21.4% |
| Intraoral Radiographs | $8.2 | $9.6 | 16.7% |
| Source: HICPS adapted by Business Support, Audit and Negotiations Division | |||
Figure 5.9: Distribution of Eligible NIHB Population, Dental Expenditures and Incidence by Age Group
2016/17
The main drivers of NIHB Dental expenditures are increased rates of utilization and increases in the fees charged for services by dental professionals. The types of dental services provided also have an impact on expenditures.
The ratio of incidence to expenditures is relatively consistent across most age groupings; however, there are notable exceptions. For children aged 0 to 9, a larger number of low-cost procedures (e.g., low-cost restorative procedures such as fillings) are provided, so this group accounts for 24.9% of claims, but only 17.6% of expenditures.
Figure 5.9: Distribution of Eligible NIHB Population, Dental Expenditures and Incidence by Age Group, FY 2016/17

Source: HICPS and SVS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Age | Eligible Clients | Expenditures | Incidence |
|---|---|---|---|
| 0-4 | 6.1% | 8.5% | 12.8% |
| 5-9 | 9.1% | 8.9% | 12.1% |
| 10-14 | 8.9% | 5.3% | 5.3% |
| 15-19 | 8.7% | 10.9% | 10.5% |
| 20-24 | 9.3% | 10.4% | 9.0% |
| 25-29 | 8.8% | 9.8% | 8.7% |
| 30-34 | 7.4% | 7.7% | 7.0% |
| 35-39 | 6.5% | 6.3% | 5.9% |
| 40-44 | 6.1% | 6.0% | 5.6% |
| 45-49 | 6.3% | 6.3% | 5.8% |
| 50-54 | 6.0% | 6.1% | 5.5% |
| 55-59 | 5.2% | 5.0% | 4.5% |
| 60-64 | 3.9% | 3.6% | 3.2% |
| 65 | 7.8% | 5.1% | 4.3% |
Section 6: NIHB Medical Transportation Expenditure and Utilization Data
In 2016/17, Non-Insured Health Benefits Medical Transportation expenditures amounted to $417.0 million or 34.5% of total NIHB expenditures. The medical transportation benefit is the second largest Program expenditure.
NIHB Medical Transportation benefits are needs driven and funded in accordance with the policies set out in the NIHB Medical Transportation Policy Framework to assist eligible clients to access medically necessary health services that cannot be obtained on reserve or in their community of residence.
NIHB Medical Transportation benefits are managed by Department of Indigenous Services regional offices, or by First Nations or Inuit Health Authorities, organizations or territorial governments who manage the benefit through contribution agreements.
NIHB Medical Transportation benefits include:
- Ground Travel (private vehicle; commercial taxi; fee-for-service driver and vehicle; band vehicle; bus; train; snowmobile taxi; and ground ambulance);
- Air Travel (scheduled flights; chartered flights; helicopter; and air ambulance);
- Water Travel (motorized boat; boat taxi; and ferry);
- Living Expenses (meals and accommodations); and
- Transportation costs for health professionals to provide services to isolated communities.
NIHB Medical Transportation benefits may be provided for clients to access the following types of medically required health services:
- Medical services insured by provincial/territorial health plans (e.g., appointments with physician, diagnostic tests, hospital care);
- Alcohol, solvent, drug abuse and detox treatments;
- Traditional healers; and
- Eligible benefits and services covered by the NIHB Program.
NIHB Medical Transportation benefits may also be provided for a medical escort (such as a nurse) to travel with a client, or so that a family member or caregiver can accompany a client who needs assistance.
In addition to facilitating client travel to appointments for these medical services, significant efforts have been made over the past few years to bring health care professionals to under-serviced and/or remote and isolated communities. These efforts enhance access to medically necessary services in communities and can be more cost effective than bringing individual clients to the service provider.
Figure 6.1: Distribution of NIHB Medical Transportation Expenditures ($ Millions)
2016/17
In 2016/17, NIHB Medical Transportation expenditures totalled $417.0 million. Figure 6.1 illustrates the components of medical transportation expenditures under the NIHB Program.
Contribution agreements for the management of medical transportation benefits by First Nations or Inuit Health Authorities, organizations or territorial governments represented the largest component, accounting for $170.1 million, or 40.8% of total benefit expenditures.
Of benefits managed by the NIHB Program, scheduled flights at $77.4 million (18.6%), living expenses at $52.7 million (12.6%) and land ambulance at $49.8 million (11.9%) were the largest expenditures, accounting for a combined total of over 40%.
Rounding out medical transportation expenditures are costs for air ambulance at $39.1 million (9.4%), land and water at $20.4 million (4.9%) and chartered flights at $7.5 million (1.8%).
Figure 6.1: Distribution of NIHB Medical Transportation Expenditures ($ Millions) 2016/17

Source: FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Expenditure | $M | % |
|---|---|---|
| Scheduled Flights | $77.4 | 18.6% |
| Air Ambulance | $39.1 | 9.4% |
| Land Ambulance | $49.8 | 11.9% |
| Chartered Flights | $7.5 | 1.8% |
| Living Expenses | $52.7 | 12.6% |
| Land & Water | $20.4 | 4.9% |
| Contribution Agreements | $170.1 | 40.8% |
| Total NIHB Medical Transportation Expenditures | $417.0M | 100.0% |
Figure 6.2: Annual NIHB Medical Transportation Expenditures
2012/13 to 2016/17
NIHB Medical Transportation expenditures increased by 10.9% in 2016/17 compared to the previous year.
Over the past five years, overall medical transportation costs have grown by 18.7% from $351.4 million in 2012/13 to $417.0 million in 2016/17. As with other benefits, expenditure growth during this period was significantly impacted by the transfer of BC clients to the FNHA in 2013.
On a regional basis, the highest growth rates over this period were in the Atlantic Region where expenditures grew by 34.9% from $6.9 million in 2012/13 to $9.3 million in 2016/17. This was followed by the Manitoba Region with an increase of 34.5% from $109.4 million in 2012/13 to $147.2 million in 2016/17.
The Manitoba Region had the highest total medical transportation expenditure at $147.2 million and had the largest net increase in expenditures over the past five years as medical transportation costs grew by $37.8 million over this period. The Ontario Region had the second largest net increase in expenditures over the past five years at $15.6 million followed by the Northern Region at $13.4 million.
*If expenditures for FNHA eligible clients are excluded from 2012/13 and 2013/14 total NIHB expenditures, then the growth rate for 2013/14 would have been 3.6%.
Figure 6.2.1: NIHB Medical Transportation Expenditures and Annual Percentage Change
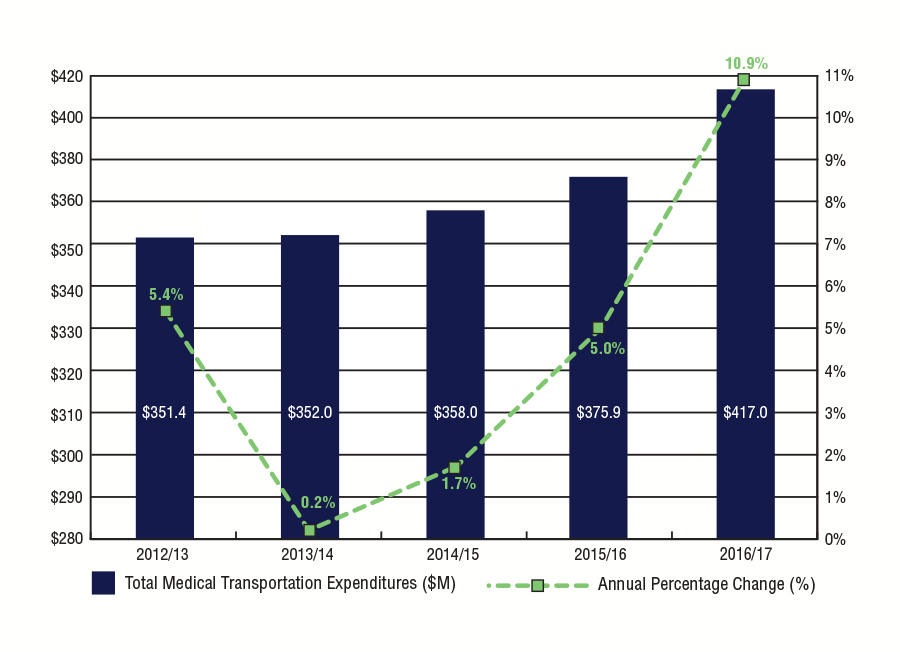
Source: FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Year | Total Medical Transportation Expenditures ($M) | Annual Percentage Change (%) |
|---|---|---|
| 2012/13 | $351.4 | 5.4% |
| 2013/14 | $352.0 | 0.2% |
| 2014/15 | $358.0 | 1.7% |
| 2015/16 | $375.9 | 5.0% |
| 2016/17 | $417.0 | 10.9% |
| Region | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|
| Atlantic | $6,875 | $6,916 | $7,419 | $8,380 | $9,277 |
| Quebec | $22,578 | $21,945 | $23,506 | $23,687 | $23,501 |
| Ontario | $59,251 | $62,865 | $65,781 | $67,772 | $74,890 |
| Manitoba | $109,409 | $111,016 | $115,705 | $125,308 | $147,167 |
| Saskatchewan | $45,793 | $47,180 | $51,543 | $53,566 | $58,902 |
| Alberta | $39,216 | $41,451 | $45,756 | $46,252 | $48,157 |
| North | $41,727 | $44,703 | $48,246 | $50,940 | $55,125 |
| Total | $351,424 | $352,036 | $357,963 | $375,904 | $417,019 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | |||||
Figure 6.3: NIHB Medical Transportation Expenditures by Type and Region ($ 000's)
2016/17
National NIHB Medical Transportation expenditures increased by 10.9% to $417.0 million in 2016/17.
The Manitoba Region had the largest percentage increase in medical transportation expenditures in 2016/17, with an increase of 17.4% from the previous fiscal year. The Atlantic Region followed with a 10.7% increase in expenditures.
In 2016/17, the Manitoba Region had the highest overall NIHB Medical Transportation expenditure at $147.2 million, primarily as a result of air transportation which totalled $74.5 million. High medical transportation costs in the region reflect in part the large number of First Nations clients living in remote or fly-in only northern communities.
The Ontario Region represented the second highest medical transportation expenditure total in 2016/17 at $74.9 million. The regions of Saskatchewan and the North followed at $58.9 million and $55.1 million, respectively.
| TYPE | Atlantic | Quebec | Ontario | Manitoba | Saskatchewan | Alberta | North | TOTAL |
|---|---|---|---|---|---|---|---|---|
| Scheduled Flights | $1,431 | $233 | $26,060 | $39,844 | $7,753 | $979 | $1,118 | $77,419 |
| Air Ambulance | $32 | $189 | $37 | $30,792 | $4,389 | $1,841 | $1,835 | $39,114 |
| Chartered Flights | $0 | $2 | $449 | $3,913 | $1,382 | $1,753 | $0 | $7,498 |
| Land Ambulance | $544 | $204 | $711 | $16,986 | $17,094 | $14,270 | $1 | $49,810 |
| Land & Water | $1,539 | $106 | $3,653 | $4,853 | $7,845 | $1,717 | $728 | $20,441 |
| Living Expenses | $824 | $18 | $18,700 | $21,791 | $6,126 | $3,915 | $1,281 | $52,654 |
| Total Operating | $4,370 | $753 | $49,608 | $118,178 | $44,589 | $24,475 | $4,963 | $246,936 |
| Total Contributions | $4,907 | $22,748 | $25,282 | $28,989 | $14,313 | $23,682 | $50,162 | $170,083 |
| Total | $9,277 | $23,501 | $74,890 | $147,167 | $58,902 | $48,157 | $55,125 | $417,019 |
| % Change from 2015/16 | 10.7% | -0.8% | 10.5% | 17.4% | 10.0% | 4.1% | 8.2% | 10.9% |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | ||||||||
Figure 6.4: NIHB Medical Transportation Contribution and Operating Expenditures by Region ($ Millions)
2016/17
Figure 6.4 compares contribution funding to operating costs in NIHB Medical Transportation. Contribution funding is provided to First Nations bands, territorial governments and other organizations to manage elements of the medical transportation benefit (e.g., coordinating accommodations, managing ground transportation, etc.), whereas operating costs are medical transportation benefits that are managed directly by Department of Indigenous Services Canada regional offices.
Manitoba Region had the largest operating expenditure for NIHB Medical Transportation in 2016/17 at $118.2 million. This higher cost in the Manitoba Region is due largely to the high number of clients living in remote or fly-in only communities in the northern areas of the province who require air travel to access health services in Winnipeg. The Ontario Region had the next largest operating expenditure at $49.6 million, followed closely by the Saskatchewan Region at $44.6 million. Together these three regions accounted for 86.0% of all operating expenditures for medical transportation.
In 2016/17, the Northern Region had the largest contribution expenditures for NIHB Medical Transportation at $50.2 million, followed by the regions of Manitoba and Ontario at $29.0 million and $25.3 million, respectively. Almost all NIHB Medical Transportation services were delivered via contribution agreements in Quebec.
Figure 6.4: NIHB Medical Transportation Contribution and Operating Expenditures by Region ($ Millions) 2016/17
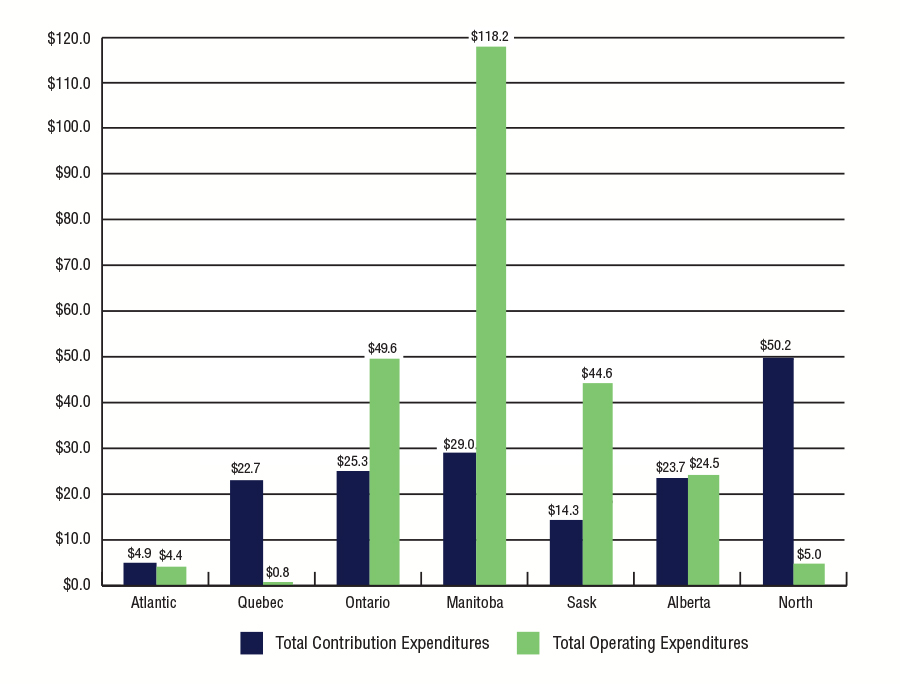
Source: FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Region | Total Contribution Expenditures ($M) | Total Operating Expenditures ($M) |
|---|---|---|
| Atlantic | $4.9 | $4.4 |
| Quebec | $22.7 | $0.8 |
| Ontario | $25.3 | $49.6 |
| Manitoba | $29.0 | $118.2 |
| Sask | $14.3 | $44.6 |
| Alberta | $23.7 | $24.5 |
| North | $50.2 | $5.0 |
Figure 6.5: NIHB Medical Transportation Operating Expenditure by Type ($ Millions)
2016/17
In 2016/17, scheduled flights represented the largest portion of NIHB's Medical Transportation operating expenditures at $77.4 million or 31.4% of the total national operating expenditures. Living expenses, which include accommodations and meals, was the second highest at $52.7 million, or 21.3% of operating expenditures. Land ambulance followed at $49.8 million or 20.2%, and air ambulance costs comprised $39.1 million or 15.8% of medical transportation operating costs.
Private vehicle expenditures ($4.2 million) are the costs reimbursed through a per-kilometre allowance for private vehicle used by a client to access eligible health services. The NIHB private vehicle kilometric allowance rates are directly linked to the National Joint Council's (NJC) Government Commuting Assistance Directive Lower Kilometric Rates.
Figure 6.5: NIHB Medical Transportation Contribution and Operating Expenditures by Region ($ Millions) 2016/17
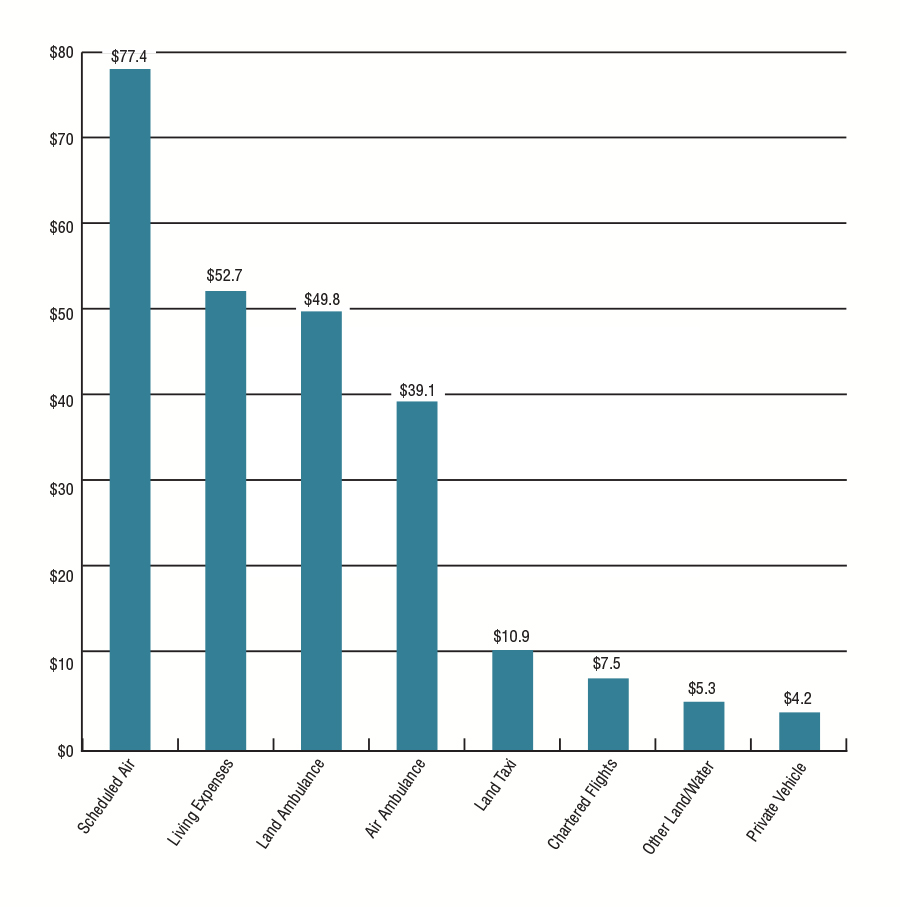
Source: FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| MT Category | Expenditure (million's) |
|---|---|
| Scheduled Air | $77.4 |
| Living Expenses | $52.7 |
| Land Ambulance | $49.8 |
| Air Ambulance | $39.1 |
| Land Taxi | $10.9 |
| Chartered Flights | $7.5 |
| Other Land/Water | $5.3 |
| Private Vehicle | $4.2 |
Figure 6.6: Per Capita NIHB Medical Transportation Expenditures by Region
2016/17
In 2016/17, the national per capita expenditure for NIHB Medical Transportation benefits was $489.
Manitoba recorded the highest per capita expenditure in medical transportation at $963, followed by the Northern Region at $803. These expenditures reflect the large number of First Nations and Inuit clients living in remote or fly-in communities that need to fly south for health services.
In contrast, the Atlantic Region had the lowest per capita expenditure at $143, a slight increase from $132 in the previous year. Compared to other regions, this lower per capita cost is reflective of the geography of the region, which allows easier access to health services with less need for air travel.
Figure 6.6: Per Capita NIHB Medical Transportation Expenditures by Region 2016/17

Source: SVS and FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Region | Per Capita Expenditures |
|---|---|
| Atlantic | $143 |
| Quebec | $331 |
| Ontario | $361 |
| Manitoba | $963 |
| Saskatchewan | $395 |
| Alberta | $398 |
| North | $803 |
| National | $489 |
Section 7: NIHB Vision Benefits, Mental Health Counselling Benefits and Other Health Care Benefits Data
In 2016/17, the total combined expenditure for NIHB Vision benefits ($32.4 million), Mental Health Counselling benefits ($21.7 million) and Other Health Care benefits ($6.0 million) was $59.8 million, or 5.0% of total NIHB expenditures for the fiscal year.
The NIHB Program provides coverage for
- Eye examinations;
- Corrective eyewear. Eligible benefits are described in the Vision Care Benefit List;
- Eyeglass repairs; and
- Other vision care benefits depending on the specific medical needs of the client.
Some items such as ocular prosthesis and low vision aids are covered by NIHB as Medical Supplies and Equipment benefits.
Vision care benefits are eligible when provided by an NIHB recognized provider (optician, optometrist or ophthalmologist), in accordance with the policies set out in the NIHB Vision Care Policy Framework and the Vision Care Benefit List. Many provincial or territorial health plans provide public coverage for eye examinations based on the client's age or medical condition, and NIHB provides coverage for other clients where needed.
NIHB mental health counselling benefits are intended to provide coverage to support individuals in significant distress in order to stabilize their condition and transition them to other mental health supports, if needed. Mental health counselling is eligible for coverage when it is provided by an NIHB recognized mental health professional such as a Registered Psychologist. The Program also works with communities to provide services to help respond to community-level crisis events.
NIHB Other Health Care includes expenditures related to funding arrangements with the FNHA for Bill C-3 and Qalipu clients, and for payment of health premiums for Inuit clients in British Columbia. Other expenditures also include funding for Program oversight and partner contribution agreements.
Figure 7.1: NIHB Vision Expenditures and Growth by Region ($ 000's)
2016/17
NIHB Vision expenditures totalled $32.4 million in 2016/17. Regional operating expenditures accounted for $27.6 million (85.3%) of total expenditures while contribution costs accounted for $4.8 million (14.7%).
In 2016/17, the Alberta Region had the highest expenditures in NIHB Vision benefits at $6.9 million, a percentage share of 21.4%, followed by the Saskatchewan Region at $6.5 million (20.2%) and the Ontario Region at $6.2 million (19.2%).
| Region | Operating | Contributions | Total |
|---|---|---|---|
| Atlantic | $3,502 | $0 | $3,502 |
| Quebec | $1,762 | $0 | $1,762 |
| Ontario | $5,670 | $552 | $6,223 |
| Manitoba | $3,879 | $326 | $4,204 |
| Saskatchewan | $6,533 | $0 | $6,533 |
| Alberta | $5,881 | $1,047 | $6,928 |
| North | $376 | $2,841 | $3,217 |
| Total | $27,604 | $4,766 | $32,370 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | |||
Figure 7.2: Annual NIHB Vision Expenditures
2012/13 to 2016/17
In 2016/17, NIHB Vision expenditures increased by 7.8% from the previous year. Over the past five years, as with other benefits, vision care expenditures declined sharply in 2013/14 and 2014/15 due to the transfer of BC clients to the FNHA, and increased in subsequent years.
On a regional basis, the highest expenditure growth rate over this five year period was in the Alberta Region where expenditures grew by 18.7% from $5.8 million in 2012/13 to $6.9 million in 2016/17. The largest net increases in expenditures over the past five years took place in the Alberta Region where total vision benefit costs grew by $1.1 million over this period, followed by the Saskatchewan Region where costs grew by $857 thousand. The significant drop in Northern Region vision expenditures in fiscal year 2014/15 is due to a change in financial coding for specific Vision benefit contribution agreements in Nunavut and the Northwest Territories.
Figure 7.2.1: NIHB Vision Expenditures and Annual Percent Change
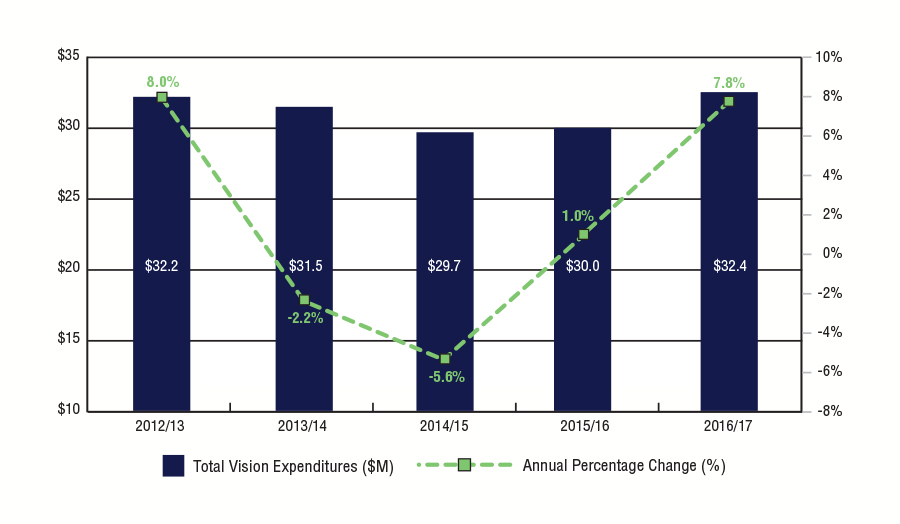
Source: FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Year | Total Vision Expenditures ($M) | Annual Percentage Change (%) |
|---|---|---|
| 2012/13 | $32.2 | 8.0% |
| 2013/14 | $31.5 | -2.2% |
| 2014/15 | $29.7 | -5.6% |
| 2015/16 | $30.0 | 1.0% |
| 2016/17 | $32.4 | 7.8% |
| Region | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|
| Atlantic | $2,969 | $2,757 | $2,666 | $3,021 | $3,502 |
| Quebec | $1,570 | $1,619 | $1,622 | $1,749 | $1,762 |
| Ontario | $5,412 | $5,721 | $5,717 | $6,160 | $6,223 |
| Manitoba | $4,048 | $4,348 | $4,800 | $4,212 | $4,204 |
| Saskatchewan | $5,676 | $5,611 | $6,066 | $6,104 | $6,533 |
| Alberta | $5,836 | $5,936 | $7,084 | $6,207 | $6,928 |
| North | $3,370 | $3,763 | $1,743 | $2,564 | $3,217 |
| Total | $28,882 | $29,755 | $29,704 | $30,017 | $32,370 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | |||||
Figure 7.3: Per Capita NIHB Vision Expenditures by Region
2016/17
In 2016/17, the national per capita expenditure in NIHB Vision benefits was $38.
Alberta had the highest per capita expenditure at $57, followed by the Atlantic Region and the Northern Region at $54 and $47 respectively. The lowest per capita NIHB Vision benefit expenditure was in the Quebec Region at $25.
Figure 7.3: Per Capita NIHB Vision Expenditures by Region 2015/16
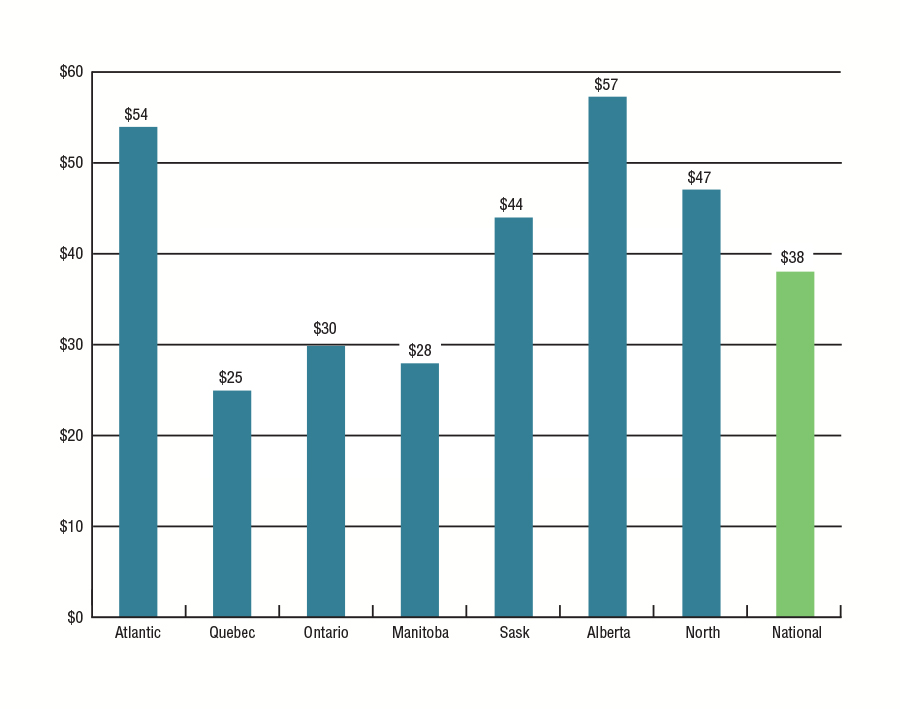
Source: SVS and FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Region | Cost per capita |
|---|---|
| Atlantic | $54 |
| Quebec | $25 |
| Ontario | $30 |
| Manitoba | $28 |
| Saskatchewan | $44 |
| Alberta | $57 |
| North | $47 |
| National | $38 |
Figure 7.4: NIHB Mental Health Counselling Expenditures by Region ($ 000's)
2016/17
Prior to 2014/15, NIHB Mental Health Counselling expenditures were reported under Other Health Care. In this edition of the NIHB Annual Report, and going forward, expenditures associated with the provision of mental health counselling services to NIHB clients will be reported separately.
In 2016/17, NIHB Mental Health Counselling expenditures amounted to $21.7 million. Regional operating expenditures accounted for $14.3 million (65.9%) of total expenditures while contribution costs accounted for $7.4 million (34.1%).
In 2016/17, the Alberta Region had the highest percentage share of NIHB Mental Health Counselling expenditures at 29.7% followed by the Manitoba and Ontario regions at 25.9% and 18.8% respectively.
| Region | Operating | Contributions | Total |
|---|---|---|---|
| Atlantic | $355 | $235 | $601 |
| Quebec | $1,093 | $199 | $1,292 |
| Ontario | $3,685 | $406 | $4,091 |
| Manitoba | $4,057 | $1,579 | $5,635 |
| Saskatchewan | $1,817 | $1,487 | $3,304 |
| Alberta | $3,310 | $3,134 | $6,444 |
| North | $0 | $362 | $362 |
| Total | $14,317 | $7,411 | $21,728 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | |||
Figure 7.5: Per Capita NIHB Mental Health Counselling Expenditures by Region ($ 000's)
2016/17
In 2016/17, the national per capita expenditure for NIHB Mental Health Counselling was $25.
The Alberta Region had the highest per capita expenditure at $53, followed by the Manitoba Region at $37 per eligible client.
Figure 7.5: Capita NIHB Mental Health Counselling Expenditures by Region ($ 000's)
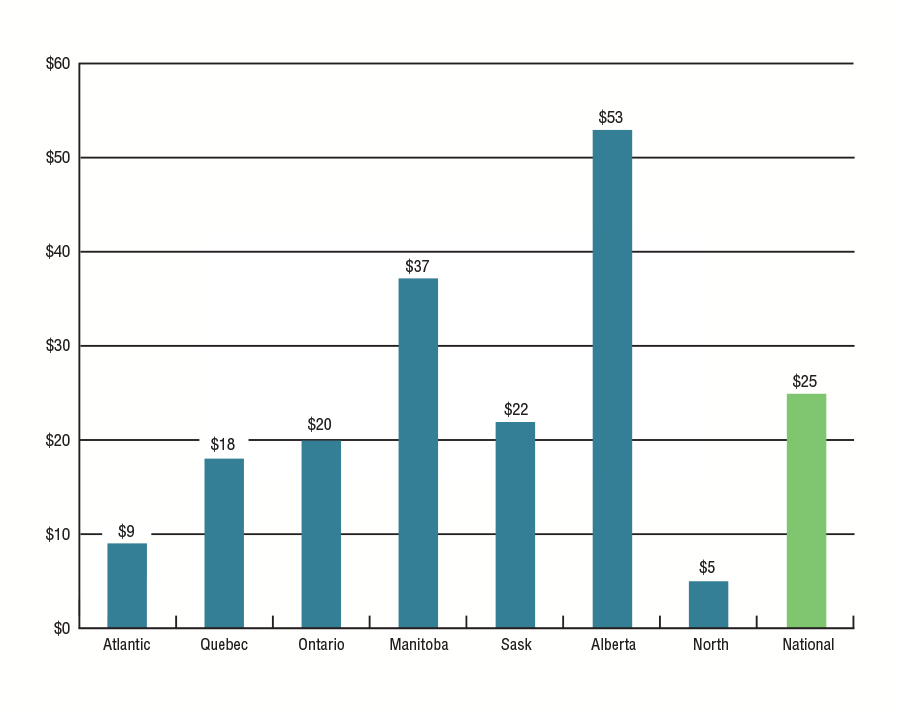
Source: SVS and FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Region | Mental Health Care Per Capita |
|---|---|
| Atlantic | $9 |
| Quebec | $18 |
| Ontario | $20 |
| Manitoba | $37 |
| Saskatchewan | $22 |
| Alberta | $53 |
| North | $5 |
| National | $25 |
Figure 7.6: NIHB Other Health Care Expenditures by Region ($ 000's)
2016/17
In 2016/17, NIHB Other Health Care expenditures totalled $6.0 million. The majority of these expenditures are related to contribution agreements including funding arrangements with the FNHA for Bill C-3 and Qalipu clients, and for payment of health premiums for Inuit clients in British Columbia.
Other expenditures in this category include contribution agreements with national client stakeholder organizations (Assembly of First Nations and Inuit Tapiriit Kanatami), as well as with regional Indigenous organizations that employ NIHB Navigators to act as a resource for communities, organizations or individuals who need assistance or information on the NIHB Program.
| Region | Operating | Contributions | Total |
|---|---|---|---|
| Atlantic | $9 | $197 | $207 |
| Quebec | $6 | $256 | $263 |
| Ontario | $4 | $250 | $254 |
| Manitoba | $0 | $240 | $240 |
| Saskatchewan | $0 | $210 | $210 |
| Alberta | $0 | $0 | $0 |
| North | $0 | $260 | $260 |
| Headquarters | $62 | $4,478 | $4,540 |
| Total | $82 | $5,892 | $5,974 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | |||
Section 8: Regional Expenditure Trends 2007/08 to 2016/17
Figure 8.1: Atlantic Region
2007/08 to 2016/17
Over the ten year period from 2007/08 to 2016/17, NIHB expenditures in the Atlantic Region were impacted by changes to the NIHB eligible client population. The creation of the Qalipu Mi'kmaq First Nation band in 2011 resulted in a 2 year surge in Atlantic Regional expenditures. As of March 31, 2017, a total of 24,745 Qalipu clients were eligible to receive benefits through the NIHB Program. The decrease in expenditures in 2013/14 can be attributed to the transfer of authority to the First Nations Health Authority for clients registered to Atlantic First Nations, but residing in British Columbia.
Annual expenditures in the Atlantic Region for 2016/17 totalled $55.1 million, an increase of 17.4% over the $50.8 million spent in 2015/16. Pharmacy expenditures in 2016/17 increased by 6.1% to $31.9 million, medical transportation costs increased by 10.7% to $9.3 million and dental expenditures increased by 8.4% to $9.6 million. Mental health expenditures increased by 43.3% and vision care expenditures increased by 15.9%.
Pharmacy expenditures accounted for more than half of the Atlantic Region's total expenditures at 57.9%. Dental expenditures ranked second at 17.4%, followed by medical transportation at 16.8%. Vision care and mental health expenditures accounted for 6.4% and 1.1% of total expenditures respectively.
Figure 8.1.1: Percentage Change in Atlantic Region NIHB Expenditures ($ 000's)
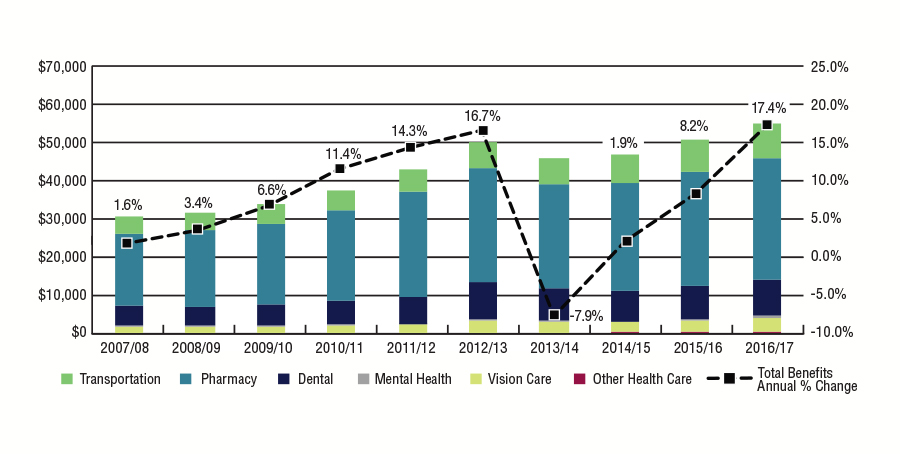
Source: FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Atlantic Region | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|---|---|---|---|---|
| Total Benefits Annual % Change | 1.6% | 3.4% | 6.6% | 11.4% | 14.3% | 16.7% | -7.9% | 1.9% | 8.2% | 17.4% |
| Atlantic Region | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|---|---|---|---|---|
| Transportation | $4,585 | $4,655 | $5,048 | $5,314 | $5,841 | $6,875 | $6,916 | $7,419 | $8,380 | $9,277 |
| Pharmacy | $18,984 | $20,119 | $21,357 | $23,689 | $27,571 | $29,979 | $27,517 | $28,398 | $30,064 | $31,899 |
| Dental | $5,204 | $4,945 | $5,426 | $6,481 | $7,164 | $9,660 | $8,609 | $8,238 | $8,846 | $9,953 |
| Mental Health | $272 | $251 | $213 | $241 | $254 | $512 | $235 | $169 | $419 | $601 |
| Vison Care | $1,495 | $1,596 | $1,612 | $1,758 | $2,021 | $2,969 | $2,757 | $2,666 | $3,021 | $3,502 |
| Other Health Care | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $21 | $44 | $207 |
| Total | $30,539 | $31,567 | $33,656 | $37,482 | $42,850 | $49,995 | $46,033 | $46,912 | $50,773 | $55,079 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | ||||||||||
Figure 8.2: Quebec Region
2007/08 to 2016/17
Annual expenditures in the Quebec Region for 2016/17 totalled $91.8 million, an increase of 8.5% from the $87.7 million spent in 2015/16.
Pharmacy expenditures increased by 7.3% to $47.4 million and dental expenditures increased by 5.6% to $17.6 million, while medical transportation costs in 2016/17 decreased slightly by -0.8% to $23.5 million. Mental health expenditures increased by 12.6% and vision care expenditures increased by 0.7%.
Pharmacy expenditures accounted for half of the Quebec Region's total expenditures in 2016/17 at 51.7%. Medical transportation expenditures ranked second at 25.6%, followed by dental at 19.1%. Vision care and mental health expenditures accounted for 1.9% and 1.4% of total expenditures respectively.
Figure 8.2.1: Percentage Change in Quebec Region NIHB Expenditures ($ 000's)
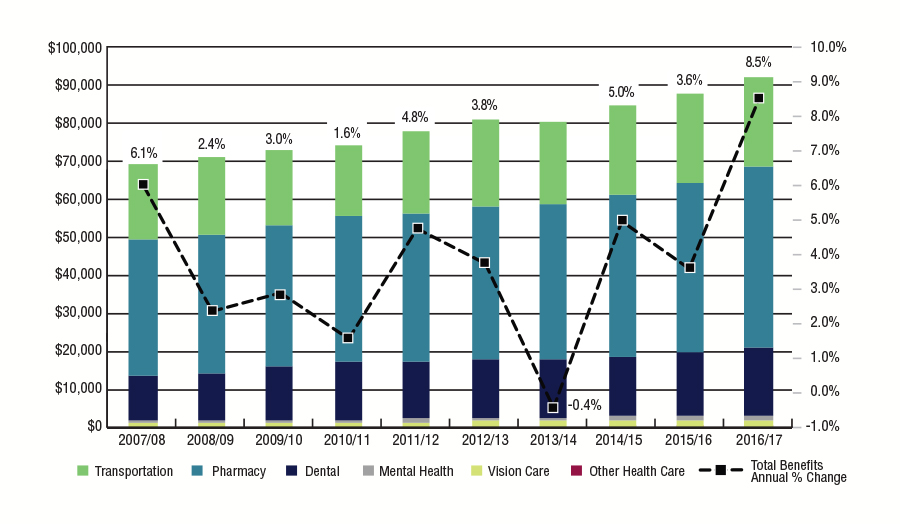
Source: FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Quebec | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|---|---|---|---|---|
| Percentage Change in Quebec Region NIHB Expenditures | 6.1% | 2.4% | 3.0% | 1.6% | 4.8% | 3.8% | -0.4% | 5.0% | 3.6% | 8.5% |
| Quebec Region | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2015/16 |
|---|---|---|---|---|---|---|---|---|---|---|
| Transportation | $20,133 | $20,502 | $19,918 | $18,943 | $21,708 | $22,578 | $21,945 | $23,506 | $23,687 | $23,501 |
| Pharmacy | $35,372 | $36,069 | $37,358 | $38,234 | $38,827 | $40,393 | $40,825 | $42,581 | $44,206 | $47,444 |
| Dental | $12,141 | $12,895 | $14,159 | $15,245 | $15,138 | $15,239 | $15,216 | $15,799 | $16,641 | $17,569 |
| Mental Health | $471 | $375 | $459 | $597 | $875 | $1,135 | $1,003 | $1,148 | $1,148 | $1,292 |
| Vison Cara | $1,257 | $1,220 | $1,280 | $1,336 | $1,404 | $1,570 | $1,619 | $1,622 | $1,749 | $1,762 |
| Other Health Care | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $10 | $258 | $263 |
| Total | $69,374 | $71,060 | $73,174 | $74,355 | $77,951 | $80,915 | $80,608 | $84,666 | $87,690 | $91,831 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | ||||||||||
Figure 8.3: Ontario Region
2007/08 to 2016/17
Annual expenditures in the Ontario Region for 2016/17 totalled $231.7 million, an increase of 14.1% from the $215.7 million spent in 2015/16.
In 2016/17, Ontario had the highest expenditures in dental care of all of the regions, at $52.1 million, an increase of 22.5%. Pharmacy expenditures in 2016/17 increased by 5.9% to $94.1 million, while medical transportation costs increased by 10.5% to $74.9 million. Vision care and mental health expenditures increased by 1.0% and 35.4% respectively.
Pharmacy expenditures accounted for 40.6% of the Ontario Region's total expenditures. Medical transportation costs ranked second at 32.3%, followed by dental at 22.5%. Vision care and mental health expenditures accounted fo 2.7% and 1.8% of total expenditures respectively.
Figure 8.3.1: Percentage Change in Ontario Region NIHB Expenditures ($ 000's)
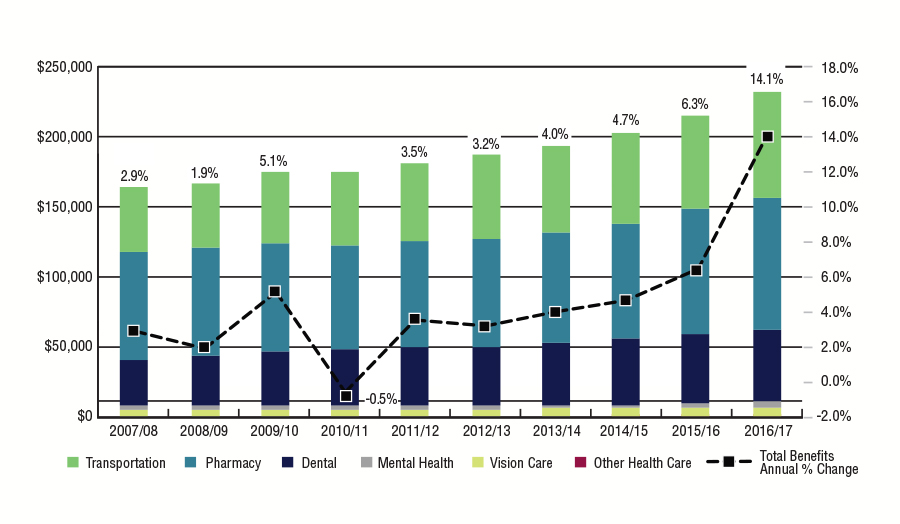
Source: FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Ontario | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|---|---|---|---|---|
| Total Benefits Annual % Change | 2.9% | 1.9% | 5.1% | -0.5% | 3.5% | 3.2% | 4.0% | 4.7% | 6.3% | 14.1% |
| Ontario Region | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2015/16 |
|---|---|---|---|---|---|---|---|---|---|---|
| Transportation | $45,618 | $46,848 | $51,889 | $52,358 | $54,725 | $59,251 | $62,865 | $65,781 | $67,772 | $74,890 |
| Pharmacy | $77,191 | $77,244 | $77,564 | $73,887 | $76,430 | $77,131 | $78,510 | $81,982 | $88,872 | $94,101 |
| Dental | $33,467 | $35,457 | $38,047 | $40,594 | $41,848 | $42,259 | $43,972 | $46,759 | $49,903 | $52,105 |
| Mental Health | $2,172 | $2,158 | $2,603 | $2,632 | $2,349 | $2,490 | $2,862 | $2,803 | $3,021 | $4,091 |
| Vision Care | $5,366 | $5,204 | $5,343 | $5,183 | $5,425 | $5,412 | $5,721 | $5,717 | $6,160 | $6,223 |
| Other Health Care | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $2 | $11 | $254 |
| Total | $163,814 | $166,910 | $175,447 | $174,653 | $180,778 | $186,544 | $193,929 | $203,043 | $215,738 | $231,663 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | ||||||||||
Figure 8.4: Manitoba Region
2007/08 to 2016/17
Annual expenditures in the Manitoba Region for 2016/17 totalled $292.0 million, an increase of 22.1% from the $258.1 million spent in 2015/16. Pharmacy expenditures in 2016/17 increased by 7.7% to $94.8 million, while medical transportation costs increased by 17.4% to $147.2 million. Dental expenditures increased by 8.8% to $40.0 million. Mental health expenditures increased by 49.1% while vision decreased by -0.2%.
Unlike most other regions, pharmacy expenditures in Manitoba do not represent the largest proportion of total expenditures. Due to the higher proportion of clients living in northern or remote communities in Manitoba, medical transportation expenditures comprised half of the Manitoba Region's total expenditures at 50.4%. Pharmacy costs ranked second at 32.5%, followed by dental at 13.7%. Vision care and mental health expenditures accounted for 2.7% and 1.8% of total expenditures respectively.
Figure 8.4.1: Percentage Change in Manitoba Region NIHB Expenditures ($ 000's)
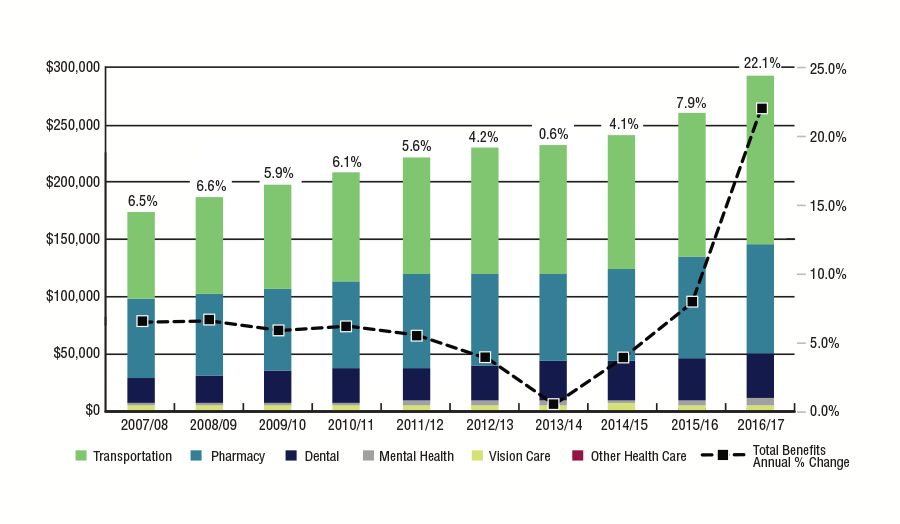
Source: FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Manitoba | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|---|---|---|---|---|
| Total Benefits Annual % Change | 6.5% | 6.6% | 5.9% | 6.1% | 5.6% | 4.2% | 0.6% | 4.1% | 7.9% | 22.1% |
| Manitoba Region | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|---|---|---|---|---|
| Transportation | $76,082 | $83,193 | $89,078 | $94,940 | $101,609 | $109,409 | $111,016 | $115,705 | $125,308 | $147,167 |
| Pharmacy | $69,317 | $71,081 | $72,789 | $76,496 | $80,639 | $80,676 | $77,034 | $81,059 | $87,997 | $94,757 |
| Dental | $21,696 | $24,444 | $26,954 | $29,399 | $29,861 | $30,734 | $33,649 | $33,527 | $36,764 | $39,986 |
| Mental Health | $2,964 | $2,619 | $3,143 | $2,930 | $3,109 | $3,429 | $3,622 | $4,099 | $3,780 | $5,635 |
| Vison Care | $2,936 | $3,157 | $3,407 | $3,612 | $3,813 | $4,048 | $4,348 | $4,800 | $4,212 | $4,204 |
| Other Health Care | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $17 | $240 |
| Total | $172,994 | $184,494 | $195,371 | $207,377 | $219,031 | $228,295 | $229,670 | $239,190 | $258,077 | $291,989 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | ||||||||||
Figure 8.5: Saskatchewan Region
2007/08 to 2016/17
Annual expenditures in the Saskatchewan Region for 2016/17 totalled $220.5 million, an increase of 22.4% from the $193.5 million spent in 2015/16.
Saskatchewan had the highest expenditures in pharmacy, followed closely by Manitoba and Ontario. In Saskatchewan, pharmacy expenditures in 2016/17 increased by 14.2% to $104.1 million, while medical transportation costs increased by 10.0% to $58.9 million and dental expenditures increased by 15.3% to $47.3 million. Vision care and mental health expenditures increased by 7.0% and 102.6% respectively.
Pharmacy expenditures comprised the largest portion of the Saskatchewan Region's total expenditures at 47.2%, medical transportation costs ranked second at 26.7%, followed by dental at 21.5%. Vision care and mental health expenditures accounted for 3.0% and 1.5% of total expenditures respectively.
Figure 8.5.1: Percentage Change in Saskatchewan Region NIHB Expenditures ($ 000's)

Source: FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Saskatchewan | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|---|---|---|---|---|
| Total Benefits Annual % Change | 6.2% | 4.4% | 7.0% | 8.5% | 5.1% | 1.3% | 3.3% | 6.7% | 7.5% | 22.4% |
| Saskatchewan Region | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|---|---|---|---|---|
| Transportation | $36,239 | $36,239 | $38,971 | $41,896 | $45,084 | $45,793 | $47,180 | $51,543 | $53,566 | $58,902 |
| Pharmacy | $60,749 | $62,809 | $66,639 | $70,625 | $73,293 | $74,646 | $78,546 | $83,361 | $91,170 | $104,082 |
| Dental | $24,636 | $28,102 | $30,777 | $35,317 | $36,941 | $36,219 | $36,399 | $37,679 | $41,028 | $47,321 |
| Mental Health | $942 | $870 | $812 | $896 | $1,499 | $1,038 | $1,017 | $1,351 | $1,631 | $3,304 |
| Vision Care | $4,126 | $4,166 | $4,222 | $4,658 | $4,449 | $5,676 | $5,611 | $6,066 | $6,104 | $6,533 |
| Other Health Care | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $4 | $210 |
| Total | $126,561 | $132,185 | $141,420 | $153,393 | $161,265 | $163,372 | $168,752 | $180,000 | $193,502 | $220,352 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | ||||||||||
Figure 8.6: Alberta Region
2007/08 to 2016/17
The decreased growth rate recorded in 2009/10 is primarily the result of the NIHB Program no longer covering provincial health premiums in the Alberta Region because the Government of Alberta eliminated Alberta Health Care insurance premiums for all Albertans as of January 1, 2009.
Annual expenditures in the Alberta Region for 2016/17 totalled $183.1 million, an increase of 15.2% from the $168.2 million spent in 2016/17. Pharmacy expenditures in 2016/17 increased by 10.4% to $77.3 million, while medical transportation costs increased by 4.1% to $48.2 million and dental expenditures increased by 11.7% to $44.3 million. Vision care and mental health expenditures increased by 11.6% and 7.3% respectively.
Pharmacy expenditures accounted for 42.2% of the Alberta Region's total expenditures. Medical transportation costs ranked second at 26.3 %, followed closely by dental at 24.2%. Vision care and mental health expenditures accounted for 3.8% and 3.5% of total expenditures respectively.
Figure 8.6.1: Percentage Change in Alberta Region NIHB Expenditures ($ 000's)
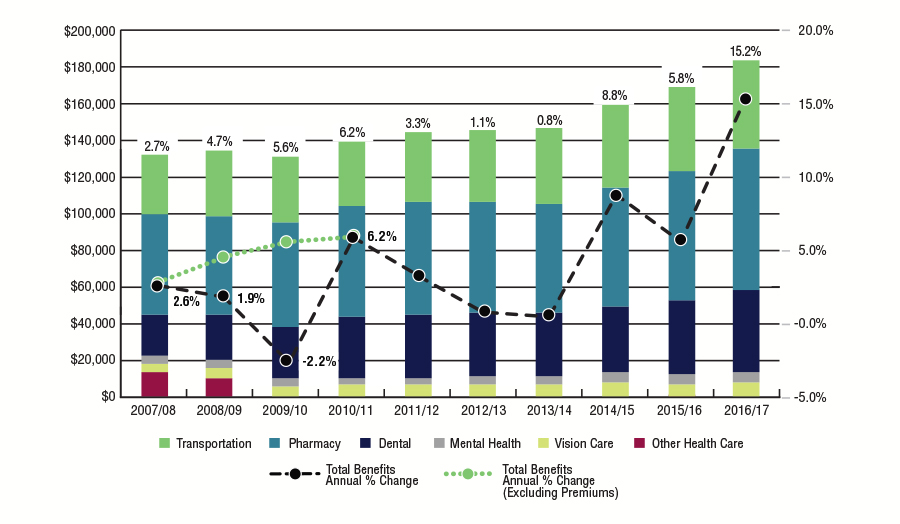
Source: FIRMS adapted by Business Support, Audit and Negotiations Division
Text Equivalent
| Alberta | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|---|---|---|---|---|
| Total Benefits Annual % Change | 2.6% | 1.9% | -2.2% | 6.2% | 3.3% | 1.1% | 0.8% | 8.8% | 5.8% | 15.2% |
| Total Benefits Annual % Change (Excluding Premiums) | 2.7% | 4.7% | 5.6% | 6.2% | 3.3% | 1.1% | 0.8% | 8.8% | 5.8% | 15.2% |
| Alberta Region | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2015/16 |
|---|---|---|---|---|---|---|---|---|---|---|
| Transportation | $32,107 | $35,357 | $36,601 | $35,877 | $37,371 | $39,216 | $41,451 | $45,756 | $46,252 | $48,157 |
| Pharmacy | $54,353 | $54,189 | $56,570 | $59,738 | $61,621 | $60,584 | $58,777 | $64,087 | $69,992 | $77,265 |
| Dental | $22,391 | $25,016 | $27,756 | $33,421 | $34,543 | $34,501 | $34,928 | $35,974 | $39,753 | $44,315 |
| Mental Health | $4,343 | $3,940 | $4,363 | $3,903 | $3,957 | $4,791 | $4,959 | $6,010 | $6,003 | $6,444 |
| Vison Care | $4,942 | $5,225 | $5,377 | $5,778 | $5,822 | $5,836 | $5,936 | $7,084 | $6,207 | $6,928 |
| Other Health Care | $12,961 | $9,920 | $0 | $0 | $0 | $0 | $0 | $0 | $3 | $0 |
| Subtotal (Excluding Premiums) | $118,135 | $123,726 | $130,666 | $138,717 | $143,313 | $144,928 | $146,051 | $158,911 | $168,208 | $183,108 |
| Total | $131,096 | $133,646 | $130,666 | $138,717 | $143,313 | $144,928 | $146,051 | $158,911 | $168,211 | $183,108 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | ||||||||||
Figure 8.7: Northern Region
2007/08 to 2016/17
Annual expenditures in the Northern Region for 2016/17 totalled $109.2 million, an increase of 15.7% from the $102.0 million spent in 2015/16.
Medical Transportation expenditures in 2016/17 increased by 8.2% to $55.1 million while Pharmacy costs increased by 3.9% to $28.5 million. Dental expenditures increased by 4.9% to $22.09 million. Vision care and mental health expenditures increased by 25.5% and 89.4% respectively.
Similar to Manitoba, Medical Transportation expenditures comprised the largest portion of the Northern Region's total expenditures at 50.5%. Pharmacy costs ranked second at 26.1%, followed by dental at 20.1%. Vision care and mental health expenditures accounted for 2.9% and 0.3% of total expenditures respectively.
Figure 8.7.1: Percentage Change in Northern Region NIHB Expenditures ($ 000's)
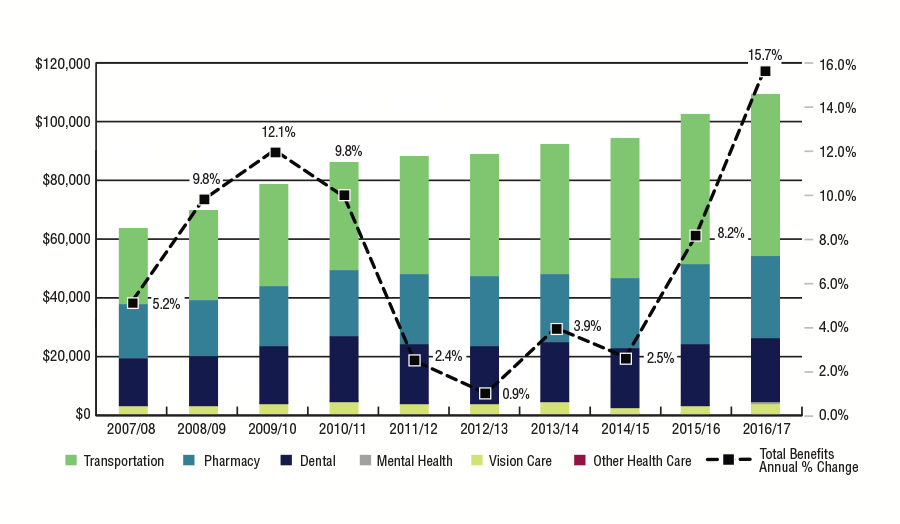
Source: Percentage Change in Northern Region NIHB Expenditures ($ 000's)
Text Equivalent
| British Columbia | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 |
|---|---|---|---|---|---|---|---|---|---|---|
| Total Benefits Annual % Change | 5.2% | 9.8% | 12.1% | 9.8% | 2.4% | 0.9% | 3.9% | 2.5% | 8.2% | 15.7% |
| Northern Region | 2007/08 | 2008/09 | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2015/16 |
|---|---|---|---|---|---|---|---|---|---|---|
| Transportation | $26,049 | $30,942 | $34,622 | $36,464 | $40,455 | $41,727 | $44,703 | $48,246 | $50,940 | $55,125 |
| Pharmacy | $18,243 | $19,073 | $20,555 | $23,190 | $23,863 | $23,682 | $23,144 | $23,941 | $27,408 | $28,488 |
| Dental | $16,752 | $16,784 | $19,627 | $22,537 | $20,079 | $19,773 | $20,415 | $20,413 | $20,936 | $21,966 |
| Mental Health | $4 | $1 | $1 | $2 | $4 | $4 | $2 | $0 | $191 | $362 |
| Vision Care | $2,380 | $2,759 | $3,284 | $3,550 | $3,387 | $3,370 | $3,763 | $1,743 | $2,564 | $3,217 |
| Other Health Care | $0 | $0 | $0 | $0 | $0 | $0 | $0 | $1 | $1 | $0 |
| Total | $63,430 | $69,649 | $78,089 | $85,744 | $87,787 | $88,557 | $92,027 | $94,343 | $102,040 | $109,157 |
| Source: FIRMS adapted by Business Support, Audit and Negotiations Division | ||||||||||
Section 9: NIHB Program Administration
Figure 9.1: Non-Insured Health Benefits Administration Costs ($ 000's)
2016/17
Figure 9.1 provides the Program administration funds expended by each region as well as NIHB headquarters (HQ) in Ottawa. In 2016/17, total NIHB administration costs were $54.0 million representing a decrease of $128 thousand over the previous fiscal year.
The roles of NIHB headquarters include:
- Program policy development and determination of eligible benefits;
- Development and maintenance of the HICPS system and other national systems such as the Medical Transportation Reporting System (MTRS);
- Audits and provider negotiations;
- Adjudicating benefit requests through the NIHB Drug Exception Centre and the Dental Predetermination Centre; and
- Maintaining productive relationships with stakeholders at the national level as well as with other federal departments and agencies.
The roles of the NIHB regions include:
- Adjudicating benefit requests for medical transportation, medical supplies and equipment, dental, vision benefits, and mental health counselling benefits;
- Working with NIHB headquarters on policy development, provider negotiations and audits; and
- Maintaining productive relationships with stakeholders at the provincial/territorial level as well as with provincial/territorial officials.
Claims processing contract costs are related to the administration of pharmacy, medical supplies and equipment and dental benefits through the Health Information and Claims Processing Services (HICPS) system, and include:
- Claim processing and payment operations;
- Claim adjudication and reporting systems development and maintenance;
- Provider registration and communications;
- Systems in support of pharmacy and MS&E benefits prior approval and dental predetermination processes;
- Provider audit programs and audit recoveries; and
- Standard and ad hoc reporting.
| Categories | Atlantic | Quebec | Ontario | Manitoba | Saskatchewan | Alberta | Northern Region | HQ | Total |
|---|---|---|---|---|---|---|---|---|---|
| Salaries | $1,344 | $1,702 | $3,620 | $2,715 | $2,931 | $3,183 | $1,146 | $11,627 | $28,266 |
| EBP | $269 | $340 | $724 | $543 | $586 | $637 | $229 | $2,325 | $5,653 |
| Operating | $93 | $61 | $367 | $58 | $111 | $130 | $77 | $2,356 | $3,254 |
| Sub Total | $1,706 | $2,104 | $4,711 | $3,316 | $3,628 | $3,949 | $1,452 | $16,308 | $37,174 |
| Claims Processing Contract Costs | $19,179 | ||||||||
| Total Administration Costs | $56,353 | ||||||||
| Source: FIRMS adapted by by Business Support, Audit and Negotiations Division | |||||||||
Figure 9.2: Non-Insured Health Benefits Administration Costs as a Proportion of Benefit Expenditures ($ Millions)
2012/13 to 2016/17
The NIHB Program is responsible for developing, maintaining and managing key business processes, systems and services required to deliver eligible non-insured health benefits. Figure 9.2 provides the percentage of NIHB Program administrative costs as a proportion of overall NIHB benefit expenditures. In 2016/17, total NIHB benefit expenditures were $1,207.5 million, of which direct benefit expenditures totaled $1,188.3 million and expenditures for claims processing administration amounted to $19.2 million. An additional $37.2 million was spent on salaries and operating costs associated with Program administration.
Total NIHB Program administration costs ($56.4 million, including claims processing and other program administration) as a proportion of direct benefit expenditures ($1.2 billion), was 4.7% in 2016/17.Over the past five fiscal years, the percentage of NIHB Program administrative costs as a proportion of total benefit expenditures has ranged from a high of 5.4% in 2014/15 to a low of 4.7% in 2016/17.
Non-Insured Health Benefits Administration Costs as a Proportion of Benefit Expenditures ($ Millions)
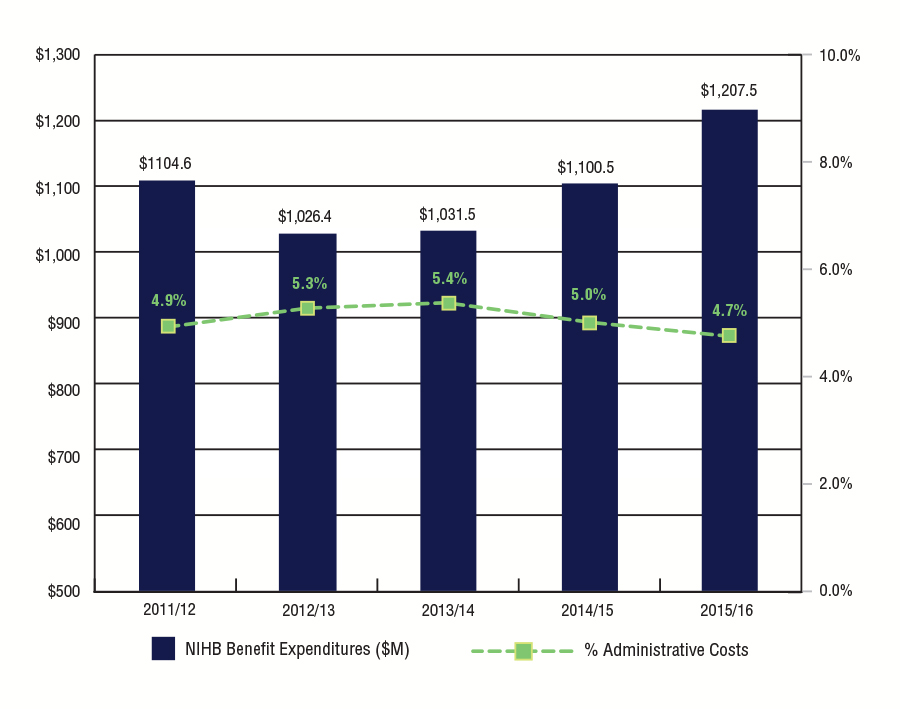
Source: FIRMS adapted by by Business Support, Audit and Negotiations Division
Text Equivalent
| Year | NIHB Benefit Expenditures ($M) | % Administrative Costs |
|---|---|---|
| 2012/13 | $1,104.6 | 4.9% |
| 2013/14 | $1,026.4 | 5.3% |
| 2014/15 | $1,031.5 | 5.4% |
| 2015/16 | $1,100.5 | 5.0% |
| 2016/17 | $1,207.5 | 4.7% |
Figure 9.3: Health Information and Claims Processing Services (HICPS)
2016/17
Claims for the Non-Insured Health Benefits (NIHB) Program pharmacy, dental and medical supplies and equipment (MS&E) benefits provided to eligible First Nations and Inuit clients are processed via the Health Information and Claims Processing Services (HICPS) system. HICPS includes administrative services and programs, technical support and automated information management systems used to process and pay claims in accordance with NIHB Program client/benefit eligibility and pricing policies.
Since 1990, the NIHB Program has retained the services of a private sector contractor to administer the following core claims processing services on its behalf:
- Claim processing and payment operations;
- Claim adjudication and reporting systems development and maintenance;
- Provider registration and communications;
- Systems in support of pharmacy and MS&E benefits prior approval and dental predetermination processes;
- Provider audit programs and audit recoveries; and
- Standard and ad hoc reporting.
The current HICPS contract is with Express Scripts Canada (formally ESI Canada). This contract came into force on December 6, 2009, following a competitive contracting process led by Public Works and Government Services Canada (PWGSC). The NIHB Program manages the HICPS contract as the project authority in conjunction with PWGSC, the contract authority.
As of March 31, 2017, there were 26,120 active providersFootnote 3 registered with the HICPS claims processor to deliver NIHB Pharmacy, MS&E and Dental benefits. The number of active providers by region and by benefit is outlined in the table below. The number of claims settled through the HICPS system is highlighted in Figure 9.3.2.
Figure 9.3.1: Number of NIHB Providers by Region and Benefit, April 2015 to March 2017
| Region | Pharmacy | MS&E | Dental |
|---|---|---|---|
| Atlantic | 783 | 221 | 1,029 |
| Quebec | 2,012 | 210 | 2,865 |
| Ontario | 3,957 | 716 | 5,900 |
| Manitoba | 420 | 81 | 745 |
| Saskatchewan | 412 | 80 | 511 |
| Alberta | 1,347 | 266 | 2,447 |
| British Columbia | 948 | 56 | 875 |
| Yukon | 8 | 10 | 48 |
| N.W.T. | 11 | 7 | 51 |
| Nunavut | 8 | 2 | 74 |
| Total | 9,926 | 1,649 | 14,545 |
| Source: HICPS adapted by Business Support, Audit and Negotiations Division | |||
Figure 9.3.2: Number of Claim Lines Settled Through the Health Information and Claims Processing Services (HICPS) System in 2016/17
Figure 9.3.2 sets out the total number of pharmacy, dental and MS&E claims settled through the HICPS system in fiscal year 2016/17. During this period, a total of 24,706.518 claim lines were processed through HICPS, an increase of 6.7% over the previous fiscal year. Ontario had the highest volume of total claims processed at 6.9 million, followed by Manitoba at 4.4 million and Saskatchewan at 4.1 million.
Claim Lines vs. Prescriptions
It is important to note that the Program reports annually on claim lines. This is an administrative unit of measure as opposed to a health care unit of measure. A claim line represents a transaction in the claims processing system and is not equivalent to a prescription. Prescriptions can contain a number of different drugs with each one represented by a separate claim line. Prescriptions for a number of drugs may be repeated and refilled many times throughout the year. In the case of repeating prescriptions, each time a prescription is refilled, the system will log another transaction (claim line). Therefore, it is possible for an individual who has a prescription that repeats multiple times in a year to have numerous related claim lines associated with the single prescription. Some prescriptions (e.g., Methadone) are dispensed daily and will increase the per capita number of claim lines.
| Region | Pharmacy | Dental | MS&E | Total |
|---|---|---|---|---|
| Atlantic | 1,377,427 | 162,082 | 39,465 | 1,578,974 |
| Quebec | 2,819,038 | 225,801 | 33,260 | 3,078,099 |
| Ontario | 6,196,148 | 614,027 | 49,653 | 6,859,828 |
| Manitoba | 3,895,755 | 460,279 | 85,143 | 4,441,177 |
| Saskatchewan | 3,459,384 | 533,665 | 84,610 | 4,077,659 |
| Alberta | 2,907,298 | 508,032 | 61,631 | 3,476,961 |
| British Columbia | 148,493 | 32,129 | 1,901 | 182,523 |
| Yukon | 107,578 | 24,255 | 3,523 | 135,356 |
| N.W.T. | 342,665 | 97,450 | 10,248 | 450,363 |
| Nunavut | 290,409 | 121,744 | 13,425 | 425,578 |
| Total Claim Lines | 21,544,195 | 2,779,464 | 382,859 | 24,706,518 |
| Source: HICPS adapted by Business Support, Audit and Negotiations Division | ||||
Figure 9.4: Benefits Management
The NIHB Program is responsible for developing, maintaining and managing key business processes, systems and services required to deliver eligible non-insured health benefits. Many items or services covered by the NIHB Program are open benefits. This means that prior approval is not required, and an enrolled provider can provide the service right away. Some items or services require prior approval from NIHB to ensure that they meet criteria for coverage.
Drug Exception Centre (DEC)
The NIHB Drug Exception Centre (DEC) was established in December 1997 to process and expedite pharmacists' requests for drug benefits that require prior approval, to help ensure consistent application of the NIHB drug benefit policy across the country, and to ensure an evidence-based approach to funding drug benefits. The DEC handles requests for prior approval from pharmacy providers across Canada.
The DEC supports the implementation of the Prescription Drug Abuse Strategy to address and prevent potential misuse of prescription drugs. The Program has set limits on medications of concern, and developed a structured approach towards client safety which includes the implementation of the Prescription Monitoring Program across the country.
The DEC is a single call centre that provides efficient responses to all requests for drugs that are not on the NIHB Drug Benefit List or require prior approval, for extemporaneous mixtures containing exception or Limited Use (LU) drugs, for prescriptions on which prescribers have indicated "No Substitution," and for claims that exceed $1,999.99.
| Status | Open Benefit (unrestricted) | Open Benefit (restricted) | Exceptions | Limited Use | Total |
|---|---|---|---|---|---|
| Total Requested | 29,194 | 10,725 | 20,334 | 67,396 | 127,649 |
| Total Approved | 28,300 | 10,226 | 17,725 | 60,219 | 116,470 |
- Open Benefit (unrestricted):
- Drugs included on the NIHB Drug Benefit List for which the total dollar value exceeds Point of Sale limit, the pre-determined frequency limit has been reached or for which more than a three-month supply is requested.
- Open Benefit (restricted):
- Drugs included on the NIHB Drug Benefit List which have been restricted due to safety concerns. These drugs are part of the Prescription Drug Abuse Strategy, such as opioids, benzodiazepines, stimulants and gabapentin.
- Exceptions:
- Drugs not included on the NIHB Drug Benefit List, as well as requests for drugs for which the physician has indicated "No Substitution".
- Limited Use:
- Drugs covered only if they are prescribed for conditions which meet specific criteria for Program coverage.
Drug Exception Centre Special Authorization Process
The Special Authorization Process for pharmacy providers has been in effect since November 2009. This program has accelerated the internal DEC process to extend medication approvals to approximately 60 additional drugs for chronic conditions.These drugs have been granted extended authorization periods beyond one year, and some will now have an indefinite authorization period, thereby facilitating access for NIHB clients and eliminating unnecessary calls by pharmacists to the DEC.
For Limited Use (LU) medications with an indefinite authorization, it is only necessary for the pharmacy provider to confirm that the client meets the clinical criteria once by obtaining a prior approval and then the client will be set up on indefinite approval.
For other drugs that continue to have a defined authorization period (i.e., 2, 3 or 5 years), a new approval must be completed according to the authorization period.
Implementing extended authorization periods for drugs used in certain chronic conditions has significantly reduced the administrative burden on pharmacy providers and enabled the DEC to deal with more complicated reviews, such as supporting the implementation of Prescription Drug Abuse Strategy.
Increased Efficiency of HICPS System to Facilitate Prior Approvals for Specific Drugs
The Health Information and Claims Processing System (HICPS) has the capacity to automatically adjudicate a number of medications to facilitate access for clients and pharmacists and to reduce calls to the DEC. For these specific drugs, the System provides a prompt to pharmacists to continue with the Prior Approval process automatically and if the pharmacists select this prompt, the request is automatically sent to the DEC for review without necessitating a call to the DEC. In this way, the DEC can immediately send a Benefit Evaluation Questionnaire (BEQ) to the physician and thereby reduce the workload of pharmacists.
Dental Predetermination Centre
The creation of a national Dental Predetermination Centre (DPC) in September 2012 has streamlined Program resources dedicated to dental benefit management, including predetermination, post-determination, client reimbursements and adjudication of appeals. Measures have been taken to simplify processes, ensure consistency in adjudication, and stabilize the workforce in the DPC. All of these measures have helped to improve processing time so that, since summer of 2014, the DPC has met the Program standard turnaround time for 10 business days to process predetermination requests. Since the creation of the DPC, NIHB has been able to remove predetermination requirements for certain dental services including:
- Replacement of complete standard dentures;
- Orthodontic examinations and diagnostic records;
- Most surgical services delivered by oral maxillofacial surgeons; and,
- Complicated tooth extractions.
Medical Supplies and Equipment Review Centre
NIHB staff at the regional level manage prior approval of medical supplies and equipment benefit requests, with support from the MS&E Review Centre (MSERC) at the NIHB national office. The Medical Supplies and Equipment Review Centre (MSERC) is staffed in-house by various administrative and health professionals, such as Registered Nurses. In cases where advice is required by a particular specialist, such as an audiologist or an orthotist, information is forwarded to the appropriate specialist consultant for review. Consultants make their recommendations based upon the current standards of practice, best practices, current scientific evidence, Program policy and recommended guidelines within their field of specialty.
Section 9.5: Claims Verification Activities
2016/17
The NIHB Program is a publicly-funded program that must account for the expenditure of those public funds. Claims verification activities contribute to the fulfillment of this overall requirement. As part of the program's risk management activities, Department of Indigenous Services Canada has mandated its claims processor to maintain a set of pre-payment and post-payment processes, including claims verification activities.
During 2016/17, the claims processor carried out claims verifications as directed by the NIHB Program. The verifications address the need of the NIHB Program to comply with accountability requirements for the use of public funds and to ensure provider compliance with the terms and conditions of the Program as outlined in the NIHB Provider Guide, Claims Submission Kit, Provider Agreement and other relevant documents. The objectives of the claims verification activities are to detect billing irregularities, to validate active licensure of providers, to ensure that services paid for were received by eligible NIHB clients and to ensure that providers retained appropriate documentation in support of each claim. Claims not meeting the billing requirements of the NIHB Program are subject to recovery.
There are four components within claims verification activities for the pharmacy, medical supplies and equipment and dental benefit areas. These are:
- Next Day Claims Verification (NDCV) Program which consists of a review of a defined sample of claims submitted by providers the day following receipt by the claims processor;
- Client Confirmation Program (CCP) which consists of a monthly mail-out to a randomly selected sample of NIHB clients to confirm the receipt of the benefit that has been billed on their behalf;
- On-Site claim verification Program which consists of the selection of a sample of claims for administrative validation with a provider's records through an on-site visit; and
- Desk claim verification Program which consists of the selection of a sample of claims for administrative validation with a provider's records. Unlike on-site verifications, a desk claim verification serves to validate records through the use of fax or mail. Generally, a smaller number of claims are reviewed during a desk audit.
Completion of the claim verification process often spans more than one fiscal year. Although the complete recovery for any verification may overlap into another fiscal year, recoveries from claims verification activities are recorded in the fiscal year in which they are received.
| Region | Dental | |||
|---|---|---|---|---|
| Audits Completed | Recoveries | NDCV/CCP Savings | Total Recoveries/ Savings | |
| Atlantic | 8 | $19,391 | $33,671 | $53,062 |
| Quebec | 1 | $2,640 | $50,161 | $52,802 |
| Ontario | 0 | $296 | $164,084 | $164,380 |
| Manitoba | 5 | $7,758 | $119,055 | $136,813 |
| Saskatchewan | 4 | $79,881 | $100,720 | $207,261 |
| Alberta | 7 | $39,187 | $154,451 | $193,588 |
| British Columbia | 7 | $163 | $258,342 | $281,245 |
| Yukon | 3 | $9,306 | $5,552 | $14,858 |
| N.W.T. | 0 | $4,963 | $18,503 | $23,466 |
| Nunavut | 8 | $47,254 | $11,545 | $58,798 |
| Total | 43 | $220,839 | $916,084 | $1,186,273 |
| Region | Pharmacy | |||
|---|---|---|---|---|
| Audits Completed | Recoveries | NDCV/CCP Savings | Total Recoveries/ Savings | |
| Atlantic | 3 | $22,185 | $49,849 | $72,034 |
| Quebec | 4 | $34,144 | $171,377 | $205,521 |
| Ontario | 5 | $73,947 | $285,030 | $358,977 |
| Manitoba | 13 | $190,671 | $155,808 | $346,478 |
| Saskatchewan | 11 | $39,739 | $55,138 | $94,876 |
| Alberta | 22 | $161,294 | $87,512 | $248,806 |
| British Columbia | 19 | $556 | $229,049 | $229,605 |
| Yukon | 1 | 0 | $1,527 | $1,527 |
| N.W.T. | 1 | 0 | $953 | $953 |
| Nunavut | 2 | $40,105 | $3,422 | $43,527 |
| Total | 81 | $562,640 | $1,039,665 | $1,602,304 |
| Region | Medical Supplies and Equipment | |||
|---|---|---|---|---|
| Audits Completed | Recoveries | NDCV/CCP Savings | Total Recoveries/ Savings | |
| Atlantic | 0 | $0 | $1,617 | $1,617 |
| Quebec | 0 | $0 | $6,025 | $6,025 |
| Ontario | 0 | $5,928 | $32,675 | $38,602 |
| Manitoba | 0 | $71,250 | $2,452 | $73,702 |
| Saskatchewan | 0 | $0 | $2,883 | $2,883 |
| Alberta | 0 | $0 | $12,273 | $12,273 |
| British Columbia | 0 | $0 | $10,751 | $10,751 |
| Yukon | 0 | $0 | $0 | $0 |
| N.W.T. | 0 | $0 | $525 | $525 |
| Nunavut | 0 | $0 | $1,200 | $1,200 |
| Total | 0 | $77,178 | $70,400 | $147,578 |
Section 10: NIHB Policy and Program Initiatives
10.1 Evidence-based Policy Development
NIHB Drug Benefit Listing and Review
NIHB Program drug benefits are based on the judgement of health professionals, consistent with the best practices of health services delivery and evidence-based standards of care. They are based on recommendations from pan-Canadian expert committees through the Canadian Agency for Drugs and Technologies in Health (CADTH) and the NIHB Drugs and Therapeutics Advisory Committee (DTAC).
As with other public drug plans in Canada, drugs considered for, or currently listed on, the Drug Benefit List (DBL) must meet minimum criteria. For example, they must be legally available for sale in Canada with a Notice of Compliance (NOC) and Drug Identification Number (DIN) or Natural Product Number (NPN), and be dispensed in a pharmacy. The drugs must also demonstrate evidence of therapeutic efficacy, safety, and incremental benefit in proportion to incremental cost.
The review process for drug products that are considered for inclusion as a benefit under the NIHB Program varies depending on the type of drug submitted. Submissions for new chemical entities, new combination drug products and existing chemical entities with new indications, must be sent to CADTH, an independent organization that provides research and information about the effectiveness of drugs and other medical treatments.
Through the Common Drug Review (CDR) and pan-Canadian Oncology Drug Review (pCODR) processes, CADTH conducts objective evaluations of the clinical, economic, and patient evidence on drugs and medical technologies. Based on this information, the CADTH expert committees provide coverage recommendations and advice to Canada's public drug plans, including the NIHB Program. The CDR and pCODR were established by federal, provincial and territorial public drug plans to reduce duplication of effort in reviewing drug submissions, to maximize the use of resources and expertise, and to enhance the consistency and quality of drug reviews.
NIHB Drugs and Therapeutics Advisory Committee (DTAC)
The NIHB DTAC is an advisory body of highly qualified health professionals who bring impartial and practical expert medical and pharmaceutical advice to the NIHB Program to promote improvement in the health outcomes of First Nations and Inuit clients through effective use of pharmaceuticals. The approach is evidence-based and the advice reflects medical and scientific knowledge, current utilization trends, current clinical practice, health care delivery and client healthcare needs.
DTAC members must hold a qualification and license in Canada as recognized health professionals with expertise in one or more areas including, but not limited to:
- Drug use evaluation/utilization
- Clinical epidemiology
- Medical or pharmacy quality assurance
- Indigenous health issues
- Health systems research
- Pharmacoeconomics
- General practice
- Geriatrics
- Pediatrics
- Drug addiction treatment or prevention
The DTAC is comprised of 8-12 core members, including First Nations or Inuit health professionals. At least three DTAC members must be physicians and at least three members must be pharmacists. The NIHB DTAC provides drug formulary listing and client safety initiative recommendations to the NIHB Program. The NIHB Program, in turn, makes listing decisions based on DTAC recommendations and other factors. More information on DTAC and its members can be found on the Drugs and Therapeutics Advisory Committee.
NIHB Oral Health Advisory Committee (NOHAC)
Established in 2016, the NIHB Oral Health Advisory Committee (NOHAC) is an independent advisory body of highly qualified oral health professionals and academic specialists who bring impartial and practical expert views, advice, and recommendations to the NIHB Program to support the improvement of oral health outcomes for First Nations and Inuit clients. The advice and recommendations provided by the Committee will follow an evidence-based approach and will reflect scientific knowledge, as well as current clinical and oral health care delivery and disease prevention best practices.
NOHAC provides professional advice on a variety of topics identified by NIHB, including NIHB dental benefit policies and criteria, best practices and evidence-based oral health disease prevention and treatment, specific clinical issues, and existing and emerging dental technologies, their use within the context of a Public Health program and their impact on oral health outcomes for the NIHB Program client population.
NOHAC members must hold a qualification and license in Canada as recognized oral health professionals (with the exception of the Health Economist and Epidemiologist), and includes both First Nations and Inuit oral health professionals. The Committee has a minimum of 8 members from the following fields of oral health care and related academic disciplines.
- Public Health Dentist
- Dental General Practitioner
- Pedodontist
- Prosthodontist
- Periodontist
- Dental Hygienist
- Health Economist
- Epidemiologist / Biostatistician
Additional members may include other types of oral health professionals such as Dental Anesthesiologist, Denturist, Oral Surgeon, Endodontist, and Orthodontist. More information on the NOHAC and its members can be found on the Non-Insured Health Benefits Oral Health Advisory Committee.
10.2 Client Safety
Pharmacy Benefit Client Safety Initiatives
Prescription drugs have the capacity to heal but also the capacity to do harm if not used correctly. Public drug plans, like the Non-Insured Health Benefits (NIHB) Program, bear a responsibility to those they serve. The NIHB Program places a high priority on client safety, and has a number of strategies in place to encourage the safe use of prescription medications.
Point of Sale (POS) Warning and Rejection Messages
The NIHB Program sends messages electronically in real-time at the POS to warn pharmacy providers about potential client safety issues including drug interactions and repeat prescriptions. Certain warning messages also require the pharmacy providers to report back with specific codes that give the Program information about the actions they have taken related to the warning code received.
The NIHB Program also sends rejection messages to pharmacists when a client's claims history indicates potential misuse or overuse of a range of prescription medications. When a rejection message is received, a pharmacy provider must contact NIHB's Drug Exception Centre (DEC), a national toll-free call centre. The DEC will provide more information to the pharmacy provider regarding the reason for coverage rejection and follow up with the prescribing physician before the Program will authorize coverage for the pharmacy benefit in question. The NIHB Program may refuse coverage for pharmacy benefits when there is evidence that suggests client safety may be at risk.
An example of a rejection message is when a client exceeds the maximum allowable quantities for acetaminophen and acetaminophen-based opioids. Clients are often unaware of the long-term consequences of commonly available acetaminophen-based products. Negative health effects can result from prolonged use, including serious liver damage if recommended dosages are exceeded.
Another example of a rejection message is a code that was created to address the health risks associated with the misuse of specific drugs of concern. These drugs include opioids (such as morphine, codeine, and oxycodone which are used to relieve pain), benzodiazepines (so-called "minor" tranquilizers, sleep aids and anti-anxiety medications) and methadone (a long-acting synthetic opioid used to treat opioid addiction or pain). In designing this warning message, it was important to recognize that all of these drugs have clinically valid applications. Therefore, the warning message was designed to focus attention on cases where there were concerns about potential misuse. This intervention addresses situations where clients access:
- 3 or more active prescriptions for benzodiazepines;
- 3 or more opioids;
- 3 or more benzodiazepines and 3 or more opioids; or
- a prescription for methadone in association with opioid-based drugs.
Trend Analysis of Prescription Drug Use
The NIHB Program analyzes broad patterns of utilization, prescribing, and dispensing on an on-going basis. This work is conducted by a team of licensed pharmacists, pharmacy technicians and experts in data analysis. Once patterns are identified, the Program intervenes to prevent the recurrence of inappropriate prescription drug use. NIHB's Prescription Drug Surveillance Strategy tracks how drugs like opioids, benzodiazepines and stimulants are prescribed and dispensed. NIHB has an electronic system that monitors claims for these drugs and lets health providers know if there is a concern. The goal of these measures is to protect client safety.
In January of 2007, NIHB launched the Prescription Monitoring Program (PMP) which focuses on potential drug use disorders related to benzodiazepines, opioids, gabapentin, and stimulant drugs. The NIHB PMP process starts by identifying clients at highest potential risk for drug use disorder for these drugs by reviewing the number of prescribing physicians (which may be an indication of "doctor shopping"), the number of pharmacy providers and the number or dose of opioids, benzodiazepines, gabapentin or stimulants claimed. Enrolment may restrict clients to a specific prescriber or prescribers in a group practice or require clients to have future claims verified and authorized by a pharmacist at NIHB's Drug Exception Centre. If the client or their health care provider cannot provide evidence to support the continuation of the drug therapy in question, the Program reserves the right to refuse coverage for the pharmacy benefit requested.
The NIHB PMP complements existing activities and promotes the optimal use of medications by allowing the Program to enhance interventions when there are concerns about how a client is using their medications. The NIHB PMP operates in all regions of Canada, with the exception of Quebec, and monitored nearly 15,000 clients in 2016-17.
Reduction in the Opioid Dose Limit
To ensure appropriate opioid use amongst NIHB clients, beginning in September 2013, the NIHB Program implemented an opioid dose limit for clients with chronic non-cancer/non-palliative pain. This limit is calculated based on the total daily dose of all opioids a client is receiving covered through the Program. This limit, which was set at 400mg of morphine equivalence per day at the beginning of 2017, will continue to gradually decrease, in line with Canadian guidelines. According to the Canadian Guideline for Safe and Effective Use of Opioids for Chronic Non-Cancer Pain published in 2010, "chronic non-cancer pain can be managed effectively in most patients with dosages at or below 200 mg/day of morphine or equivalent. Consideration of a higher dosage requires careful reassessment of the pain and of risk for opioid use disorder, and frequent monitoring with evidence of improved patient outcomes."
Coverage of Naloxone
In addition to methadone, Suboxone, and Kadian to treat opioid use disorder, the NIHB Program covers injectable naloxone, a medication that can temporarily reverse the toxic effects of opioid drugs (e.g. heroin, morphine, fentanyl). Medical help is still required after administration of naloxone. To improve access to this life saving medication, the Program added naloxone and naloxone with administration supply (kit) as an open benefit on the Drug Benefit List. Individuals at risk of opioid toxicity and people close to them are encouraged to have a naloxone kit on hand, and the training to use it.
Dental Benefit Client Safety
One of the objectives of the NIHB Program dental benefit is to provide dental services based on evidence-based standards of care and professional judgment, consistent with current best practices of health services delivery.
The NIHB Sedation and General Anaesthesia Policy is one example of the Program's commitment to client safety. Sedation and general anaesthesia services must be provided in conjunction with eligible dental services and require predetermination under the NIHB Program, in other words, approval prior to commencement of treatment. Coverage for sedation and general anaesthesia services is provided with a frequency of once in any twelve month period. In extenuating circumstances, additional sessions would be considered for coverage. This policy, while respecting the professional expertise of dental providers, encourages the minimal risk approach to the use of sedation and general anaesthesia in conjunction with associated dental services.
Section 10.3: Client and Provider Communications
The Non-Insured Health Benefits (NIHB) Program is continually seeking ways to improve communications with clients, providers and stakeholders regarding benefit coverage and administration.
The NIHB Program regularly produces newsletters and updates to inform clients and providers about any changes to NIHB policy and benefit coverage information. For example, NIHB enrolled providers for Dental, Pharmacy and Medical Supplies and Equipment receive policy updates and relevant information regarding benefits through both quarterly Provider newsletters and fax broadcasts.
The Provider newsletters are distributed to enrolled providers by Express Scripts Canada (ESC), Health Canada's claims processing contractor, and are available via the ESC website.
The NIHB website is a key venue for disseminating Program information. NIHB Program updates are produced quarterly to provide information for clients regarding changes to benefit coverage. They can be found on the Canada.ca website , and are promoted through social media on Health Canada's Healthy First Nations and Inuit Facebook Page. NIHB develops additional posts for the Healthy First Nations and Inuit Facebook page that promote client awareness of their benefit coverage. Often these posts are planned in conjunction with broader public health promotion campaigns (such as, a post on diabetes awareness will include a reminder about NIHB coverage of diabetes medications and supplies, and a post on vision health that will include a reminder about NIHB coverage of eye exams).
NIHB strives to be accessible and responsive to clients. Clients can contact NIHB directly by calling Health Canada regional offices, or the NIHB Dental Predetermination Centre. In 2016, NIHB implemented new ways for clients to contact the Program on-line: the "Contact Us" web page for the NIHB Program now provides an email address for direct inquiries to the NIHB Program, and the NIHB "Feedback Form" enables clients to inquire or send feedback directly to the Program.
Section 10.4: NIHB Navigators
NIHB Navigators help eligible clients to 'navigate' and access the NIHB Program. They are a resource for communities, organizations or individuals who need support or information on NIHB-related issues. Navigators are employed by regional Indigenous organizations. Their roles and activities are adapted to meet regional needs, and generally include the following:
- Increase understanding of the NIHB Program and share information on eligible benefits;
- Help clients and communities to resolve NIHB-related issues;
- Link with health departments and agencies to help improve client access to NIHB benefits and related health services.
Section 10.5: Collaboration with First Nations and Inuit Partners
In 2014, the Minister of Health agreed to undertake a multi-year Joint Review of the NIHB Program in partnership with the Assembly of First Nations. The overall objective of the review is to identify and implement actions that enhance client access to benefits, identify gaps in benefits, streamline service delivery to be more responsive to client needs, and increase Program efficiencies. The Joint Review is guided by a Steering Committee comprised of First Nations and FNIHB representatives. An implementation plan for changes and improvements to the NIHB mental health counselling benefit was finalized in 2015. In 2016/17 NIHB implemented numerous changes as a result, including improvements to provider enrolment and claim forms, and updating the benefit policy guide to clarify eligibility of group and family counselling.
Reviews of other benefits are underway, and NIHB prepared administrative profiles of the dental, pharmacy and vision care benefits to support the work of the Joint Review. AFN conducted a robust program of client, provider and stakeholder engagement activities to gather broad input and perspectives that will inform recommendations for Program improvements.
Health Canada continues to work with Inuit representatives through the Inuit NIHB Senior Bilateral Committee (INSBC) to identify and address areas of concern and recommendations to improve the quality, access, and delivery of NIHB benefits to Inuit clients. NIHB updates Inuit partners regularly on progress made to advance INSBC priority issues, including working towards the implementation of NIHB Navigator positions for Inuit clients in Nunavut and the Inuvialuit Settlement Region.